Cardiovascular Magnetic Resonance Study Shows PEA Able to Reverse RV Afterload in CTEPH
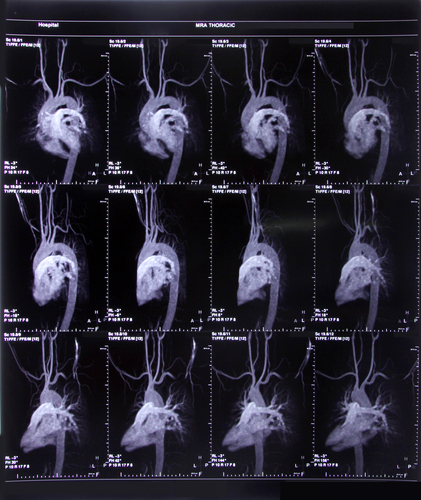
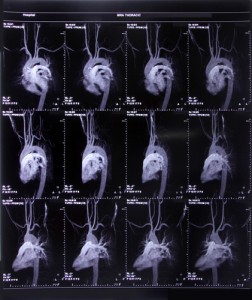 Findings from a study entitled “Right ventricular adaptation to pulmonary pressure load in patients with chronic thromboembolic pulmonary hypertension before and after successful pulmonary endarterectomy — a cardiovascular magnetic resonance study,” were recently published in the Journal of Cardiovascular Magnetic Resonance.
Findings from a study entitled “Right ventricular adaptation to pulmonary pressure load in patients with chronic thromboembolic pulmonary hypertension before and after successful pulmonary endarterectomy — a cardiovascular magnetic resonance study,” were recently published in the Journal of Cardiovascular Magnetic Resonance.
Chronic thrombolic pulmonary hypertension (CTEPH) arises from repeated or unresolved pulmonary embolisms — clots in the pulmonary arteries — and is one of the one of the leading causes of severe pulmonary hypertension and right side heart failure. With an incidence of nearly 4%, CTEPH in contrast to pulmonary hypertension of other etiologies is the only type of pulmonary hypertension that is potentially curable. Evidence shows that after a successful pulmonary endarterectomy (PEA), pulmonary vascular hemodynamics can return to normal.
[adrotate group=”4″]
When found in later stages, CTEPH involves the heart vasculature causing an increase in pulmonary arterial pressure (mPAP) and resistance (PVR), which leads to hemodynamic changes and remodeling of the right ventricle (RV). However, RV has the ability to undergo reverse remodeling after PEA. A decline in RV function is usually assessed by cardiovascular magnetic resonance (CMR), which allows full coverage of the RV. An increase in the RV afterload precedes RV function decline. In the early stages of CTEPH, contractile properties of the RV compensate for this increase in afterload, however, this compensation is insufficient, which causes RV function to decrease.
[adrotate group=”3″]
The team of researchers from Germany, led by Andreas Rolf, characterized RV adaptation to varying loading conditions in a sample of 65 patients who were assessed by CMR before and after PEA surgery. The researchers combined cine-cardiac CMR and hemodynamic data from routine right heart catheterization to determine how the RV adapts to increased afterload, and what role RV afterload plays in the reverse remodeling of the RV.
Results revealed that PEA is able to reverse RV afterload in CETPH. Furthermore, findings show that RV function is afterload dependent and that it can return to normal once normal pulmonary arterial afterload decreases and ventriculo-arterial coupling of the RV is restored. The authors also suggest that CMR in combination with RHC measurements are a good method to examine RV properties in the follow up of PH patients.