TAVI Heart Valve Surgery Has Fewer Complications for PH Patients, Analysis Shows
In patients with pulmonary hypertension (PH) with aortic stenosis — when the heart’s aortic valve fails to properly close/open — undergoing a transcatheter aortic valve implantation (TAVI) surgical procedure resulted in fewer cardiac, respiratory and bleeding complications, according to a new study.
The study “The Outcomes of Pulmonary Hypertension Patients With Severe Aortic Stenosis Who Underwent Surgical Aortic Valve Replacement or Transcatheter Aortic Valve Implantation” was published in The American Journal of Cardiology.
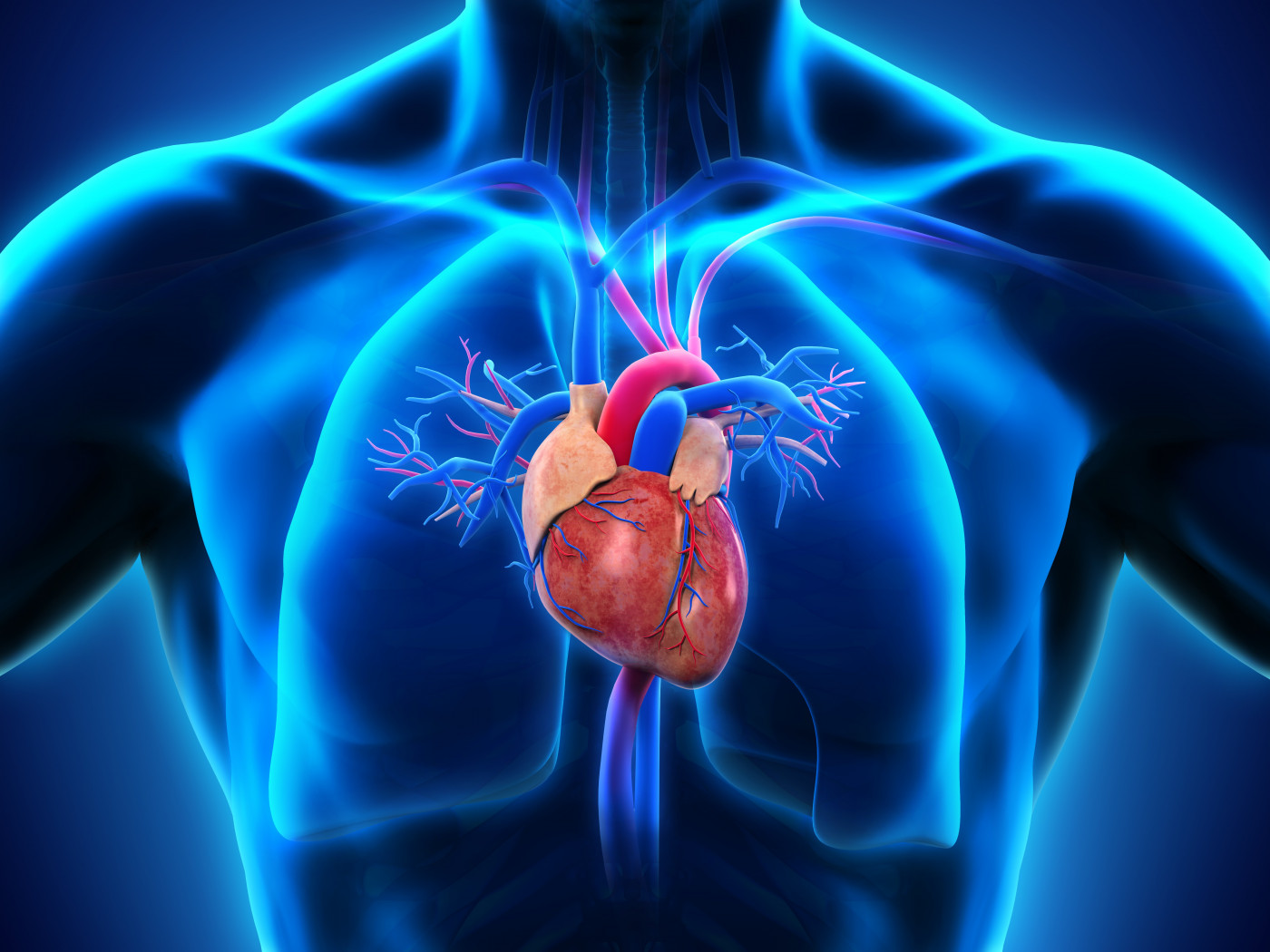
When the aortic valve, which is in the left side of the heart, becomes narrowed and stiff, it fails to open and close properly, making it more difficult for the heart to pump blood to the rest of the body. This condition is called aortic stenosis, and typically it can be treated treated with two different surgical approaches: TAVI or surgical aortic valve replacement (SAVR).
PH is a known mortality risk factor in people undergoing SAVR, which is an invasive surgery.
TAVI is another medical strategy for patients with aortic stenosis who are not fit to undergo SAVR. In TAVI, a catheter is inserted into a blood vessel in the upper leg or chest, and is moved toward the aortic valve. The catheter is then used to guide and replace the existing valve with a new tissue valve, which is placed over the top of the existing one.
The outcomes of patients with PH who undergo either TAVI or SAVR, and whether one procedure is better than the other, is unknown.
To understand the benefits and detrimental outcomes between both procedures, a research team performed a retrospective analysis of 36,786 patients with PH who underwent aortic valve surgery in U.S. hospitals from 2011 to 2014. Researchers used the National Inpatient Sample database, which contains hospital discharges in the U.S., to identify these patients.
The majority of the patients analyzed (74%, 27,225 people) underwent SAVR, while 26% submitted to TAVI (9,560 people).
The TAVI group included more women (53.2% vs 45.4%), and older patients (81.0 vs 68.5 years), compared with the SAVR group. It also had fewer African-American patients (4.6% vs 8.3%).
Results showed that PH patients in the TAVI group had a significantly higher prevalence of heart and vascular diseases, including coronary artery disease, a prior story of stroke, transient loss of blood flow (ischemia), as well as chronic pulmonary disease and renal failure, compared to the SAVR group.
PH patients showed no statistically significant difference in in-hospital mortality between the two procedures — 5.6% with TAVI, and 4.6% with SAVR.
However, TAVI patients were significantly less likely to experience cardiac complications (15.4% vs 19.9%), respiratory complications (12.4% vs 25.1%), or of needing blood transfusions (10.8% vs 24.0%), compared to the SAVR group.
In contrast, patients in the TAVI group had a higher incidence of vascular complications (4.0% vs 1.7%).
Overall, “in this observational study, patients with PH and severe symptomatic AS [aortic stenosis] who underwent TAVI had comparable in-hospital mortality and lower cardiac complications, respiratory complications, and bleeding complications compared with patients who underwent SAVR,” the team concluded.







