Echocardiography May Be Easier Way to Predict Outcomes in PAH Patients
Written by |
Measuring right ventricular (RV) function in patients with pulmonary arterial hypertension (PAH) using echocardiography is useful to predict patients’ prognosis, according to researchers at the Fondazione IRCCS Policlinico San Matteo in Italy. This may be of clinical relevance because echocardiography is cheaper and provides faster results than standard techniques, such as cardiac magnetic resonance (CMR) and radionuclide angiography.
The study, “Prognostic value of TAPSE after therapy optimisation in patients with pulmonary arterial hypertension is independent of the haemodynamic effects of therapy,” was published in the journal Open Heart.
RV function is a known determinant of morbidity and mortality in PAH patients. However, most studies that assess PAH treatment efficacy focus on changes on pulmonary vascular resistance. Few have evaluated the effects of treatment on changes in RV function, and on how that affects a patient’s prognosis.
Importantly, a number of studies report that changes in vascular resistance may not predict long-term outcome, since RV dysfunction may progress despite treatment-induced decrease in vascular resistance. Recently, imaging right ventricular structure and function by CMR has helped to stratify the prognosis of PAH patients.
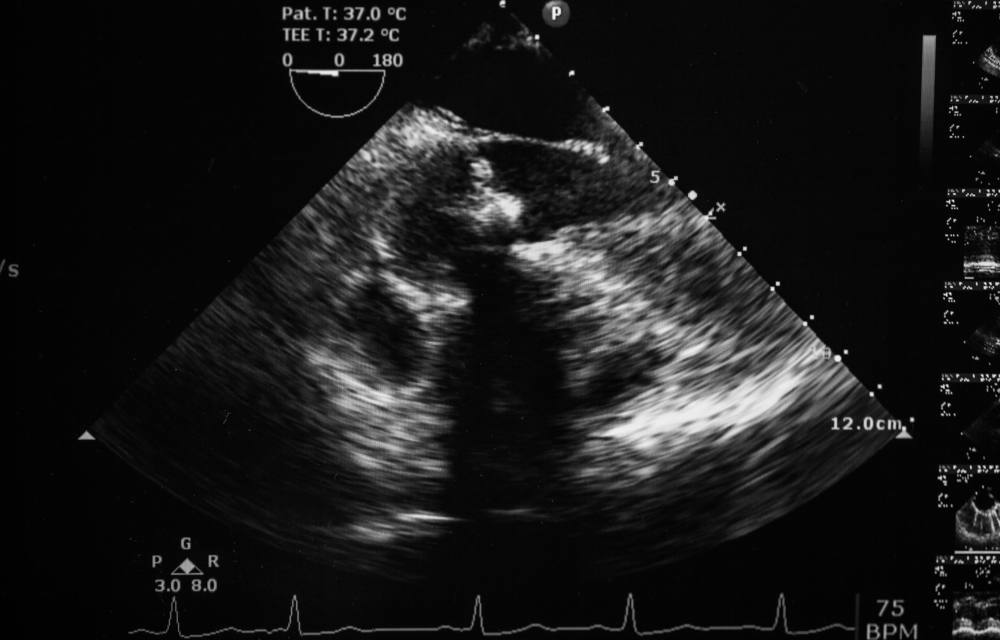
Echocardiography is not as accurate as CMR in the evaluation of RV structure and function. Its clinical relevance resides in it being a more accessible and simpler technique than CMR and radionuclide ventriculography.
In this study, the research team addressed whether a simple echocardiographic measure of RV function, called tricuspid annular plane systolic excursion (TAPSE), was able to predict patients’ prognosis following PAH therapy.
The team examined 81 patients with PAH, 33 of whom were naive to treatment, and 48 who were already under PAH treatment. Researchers found that low TAPSE, or higher RV dysfunction, at baseline was associated with a threefold increase in risk of death. Consistently, after treatment, patients with high TAPSE values had a 70 percent decrease in the risk of death or clinical worsening.
As suggested by previous studies, reduced vascular resistance after treatment was not associated with better patient outcomes. This suggests that the drugs used to treat PAH decrease pulmonary artery resistance but have a relatively modest effect on RV function, and the need exists for therapies that target both.
Nonetheless, TAPSE values were found to be good prognostic indicators for PAH-targeted therapies, and may be of help in therapeutic decision-making processes.



