Researchers Identify Biomarker in Helping Curtail PAH Caused By Scleroderma Progression
Written by |
 Pulmonary Arterial Hypertension (PAH) is a frequently encountered complication of Systemic Sclerosis (SSc). PAH is also the leading cause of morbidity and mortality among SSc patients. Despite some progress in new detection methods, standard right heart catheterization still remains the most effective means of diagnosis of PAH with Systemic Sclerosis. However, the need for the detection of biomarkers in blood and serum at early stages of the disease still remains unmet. If researchers can solve this particular diagnostic need, it could significantly aid in the early-stage detection of SSc and prevent progressive deterioration.
Pulmonary Arterial Hypertension (PAH) is a frequently encountered complication of Systemic Sclerosis (SSc). PAH is also the leading cause of morbidity and mortality among SSc patients. Despite some progress in new detection methods, standard right heart catheterization still remains the most effective means of diagnosis of PAH with Systemic Sclerosis. However, the need for the detection of biomarkers in blood and serum at early stages of the disease still remains unmet. If researchers can solve this particular diagnostic need, it could significantly aid in the early-stage detection of SSc and prevent progressive deterioration.
The circulation of Plasmacytoid Dendritic Cells — otherwise known as pDCs, a subpopulation of innate, peripheral blood mononuclear cells found in peripheral lymphoid organs — in patients with SSc have been found to secrete a protein, CXCL4 (a chemokine) in excess, according to research carried out at The University Medical Center, Utrecht, the Netherlands (as mentioned in a report in the online version of New England Journal of Medicine, December 18, 2013.) CXCL4 has thus been assumed as a direct link (clinical biomarker) for both SSc and PAH — a much awaited finding for the medical community. Now, this connection offers the potential for developing a therapeutic target for SSc.
[adrotate group=”4″]
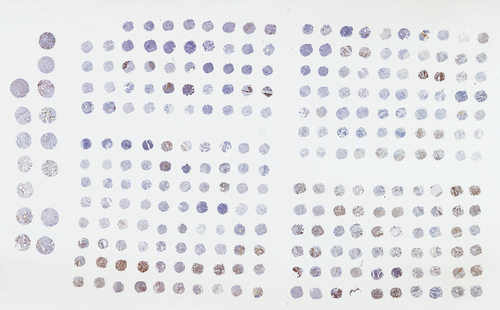
Proteomic analysis of the pDCs was conducted in those derived from SSc patients and compared against normal healthy controls. In order to check for the clinical significance of CXCL4 in SSc, it was compared against those in patients with Systemic Lupus Erythematosus (SLE), Ankylosing Spondylitis (AS), and hepatic fibrosis (HF). Further, the effects of high levels of CXCL4 were studied in-vitro and in-vivo.
Mean levels of CXCL4, as obtained from this study, were as follows: for SSc, they were as high as 25,624 pg/mL, as compared to a mere 92.5 pg/mL in control patients; 1346 pg/mL in patients with SLE; 1368 pg/mL in patients with AS; and 1668 pg/mL in patients with liver fibrosis. Now, being inflammatory conditions, high levels of CXCL4 were expected, but the figures obtained from patients with SSc was unexpected, according to the researchers. Furthermore, levels of CXCL4 also correlated with skin and lung fibrosis, as well as PAH.
[adrotate group=”3″]
Commenting on the efficacy of detecting CXCL4 levels in patients, Dr. Radstake said in an interview to Medscape, “CXCL4 is associated with the progression and clinical phenotype of SSc, and thus provides a tool for clinicians to identify those patients in need of aggressive therapy and … to avoid unnecessary side-effects for those who have mild disease. Moreover, the identified roles for CXCL4 in SSc spark our knowledge of the pathogenic pathways in this terrible condition. Now, we and other groups will have to further unravel the precise roles for CXCL4 in SSc and possibly other fibrotic and immune-mediated conditions.” He further added, “The clinical relevance of this work is pretty high, as there is no current effective therapy available for SSc. Also, there are no biomarkers [that] are able to predict which patient will have severe disease or those who will not. This is important, since therapy that is available as kind of last resort for these patients (eg, cyclophosphamide or autologous stem cell transplantation) has a high rate of mortality and/or morbidity. We definitely believe that CXCL4 might be a novel target and the first to really tackle the underlying problem that drives this terrible disease. There are multiple efforts underway to further develop CXCL4 as a clinical target for therapeutic intervention.”
Dr. Jessica Gordon, M.D. assistant attending physician in rheumatology at the Hospital for Special Surgery and assistant professor of medicine, Weill-Cornell Medical College, New York City, although not a part of this particular study, has been involved in similar lines of work. She was also of the opinion that, “CXCL4 is antiangiogenic, and patients with scleroderma have a decrease in vascular density despite the presence of other proangiogenic factors. CXCL4 upregulates fibrosis. It makes sense that a cytokine with these properties. This speaks to the likelihood that other factors are important in the development of this condition, and that it is not [due to] elevations of CXCL4 alone,” she said. “Taken together, the observations of these authors suggest an important role for CXCL4 and plasmacytoid dendritic cells in SSc in the context of other factors as well.”
Dr. Gordon’s concluded that, “It is interesting to note that there are a large number of authors from several different institutions and several different countries. In rare diseases like scleroderma, collaborative efforts like this one are very important in order for sufficient numbers of patients to be studied and to draw on the respective expertise of different centers. It is important for such collaboration to continue to be fostered in the scientific community.”
The lead authors for this study included Lenny van Bon, MD, from the Arthritis Center, Boston University School of Medicine, Massachusetts, and the Department of Rheumatology and Clinical Immunology and the Laboratory of Translational Immunology, University Medical Center Utrecht, the Netherlands; Dr. Timothy R.D.J. Radstake, MD, PhD, staff rheumatologist and head of translational immunology in the Department of Rheumatology and Clinical Immunology, University Medical Center Utrecht; and colleagues. Funding was provided jointly by the Netherlands Organization for Scientific Research, European Research Council and the Dutch Arthritis Foundation.



