IGF1 ID’d as possible target to treat pulmonary hypertension, fibrosis
Researchers screened common key genes, immune features in both diseases
Written by |
The gene coding for insulin-like growth factor 1 (IGF1) may be involved in both pulmonary hypertension (PH) and pulmonary fibrosis (PF), offering a potential target for treating both diseases, a study suggests.
That’s important because for many people with both PH and PF, a lung transplant may be the only option to bring long-lasting benefits.
The study, “Identification of the shared gene signatures between pulmonary fibrosis and pulmonary hypertension using bioinformatics analysis,” was published in Frontiers in Immunology by researchers in China.
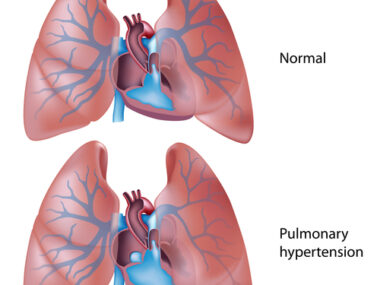
PH is high blood pressure in the blood vessels that supply the lungs. It happens when they become narrowed or blocked, restricting blood flow. The disease often occurs with PF, which is marked by lung scarring.
In idiopathic pulmonary fibrosis (IPF), where the cause of lung scarring is unknown, “8%-15% of patients have PH at diagnosis, and the prevalence is raised to 30%-50% in the advanced stage and [more than] 60% at the end stage of the disease,” the researchers wrote, noting, while the two diseases share features — such as remodeling, or abnormal repair and overgrowth of tissue in the lungs and lining the blood vessels — medications that target both PH and PF aren’t effective and may be harmful.
What genes do PH, PF have in common?
Using bioinformatics, the researchers sought to screen common key genes and immune features of PF and PH to find new therapeutic targets for both. Bioinformatics help give meaning to large sets of biological data.
They first sought to understand how different genes work together by measuring the strength of their relationships. This helps understand what genes play a role in specific diseases.
The sets (GSE53845 and GSE113439) were from the Gene Expression Omnibus public repository and included data from lung tissue samples of 40 people with IPF, 15 people with pulmonary arterial hypertension (PAH), and 19 people without these diseases who served as controls.
A total of 313 genes were found to play a role in both IPF and PAH. They were mostly involved in lymphocyte activation, which occurs when two types of immune cells called B-cells and T-cells are triggered by harmful invaders.
When the researchers zeroed in on which types of immune cells were most abundant in those samples, they identified memory CD4 T-cells, which remember past invaders to quickly fight them off.
They then sought to identify differentially expressed genes, those that are more active (upregulated) or less active (downregulated), in two other sets (GSE110147 and GSE15197) of genetic data from people with IPF, PAH, and controls.
From the thousands of genes found differentially expressed in the two databases, 197 overlapped, suggesting they may be involved in both diseases; 165 were upregulated, 32 were downregulated.
The role of IGF1 in PH, PF
Among the eight key genes in the IPF-PAH overlap was IGF1, which is important for immune cells. It’s also more active in many lung cells, including fibroblasts, which form scar tissue.
To see if IGF1 could be a therapeutic target, the researchers used siRNA, a short string of RNA that can block the production of proteins from genetic information.
Under exposure to reduced oxygen, or hypoxia, they grew pulmonary microvascular endothelial cells, which line the walls of the smallest blood vessels in the lungs. Hypoxia causes these cells to multiply.
When treated with siRNA against IGF1, the pulmonary microvascular endothelial cells grown under hypoxia didn’t multiply as much or survive as long, indicating that “knocking down IGF1 could significantly reduce [their] proliferation and apoptosis [death] resistance.”
Similar observations were made with pulmonary smooth muscle cells, which can contract around the walls of blood vessels in the lungs, and fibroblasts grown in the lab with growth factors.
Using molecular docking, a computer tool that predicts how small molecules interact with their targets, it was found that deslanoside, flavitan, ivermectin, and posaconazole may target the IGF1 protein “with strong binding activity.”
“These data findings provide a basis for future research and new potential therapeutic targets for the future treatment of PF and PH,” the researchers said.