Innovative Ultrasound Technology Allows Early Detection of PAH in Systemic Sclerosis Patients
Written by |
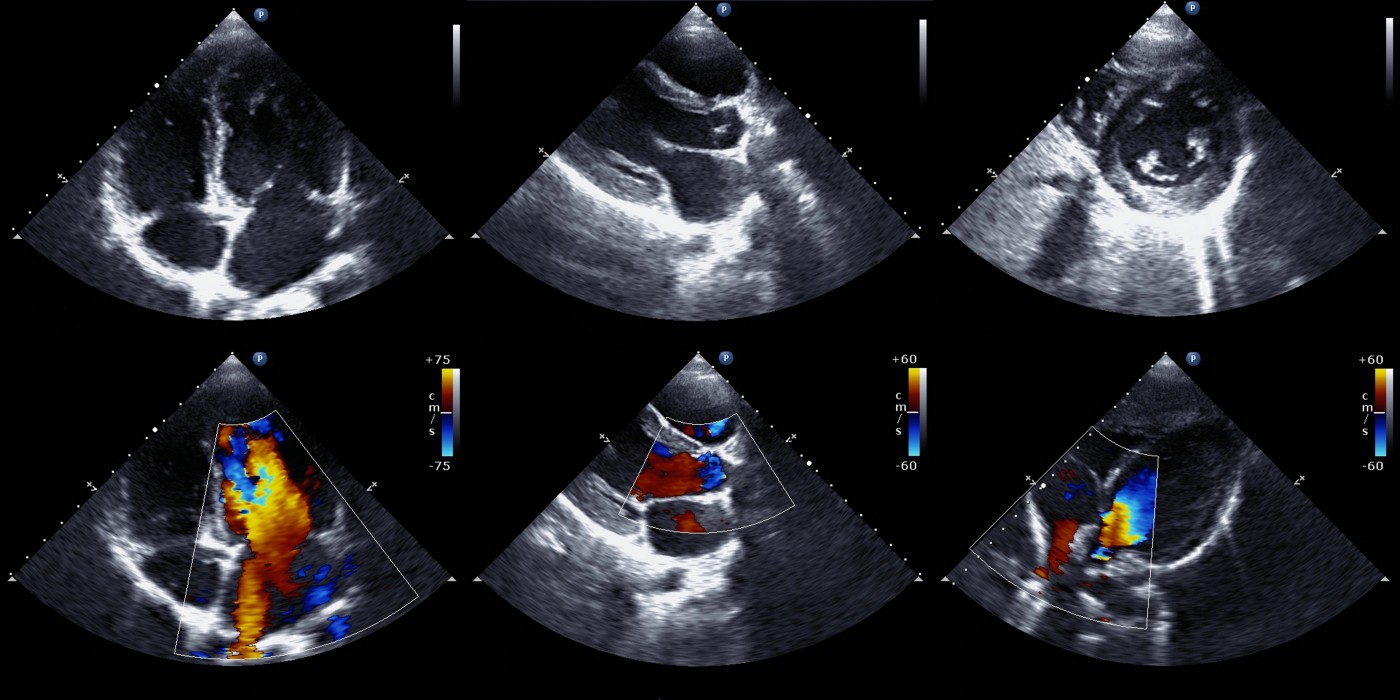
An international team led by researchers at the University Hospital Heidelberg in Germany recently revealed that stress-doppler-echocardiography, a procedure based on ultrasound technology, is effective in early detection of pulmonary arterial hypertension in patients with systemic sclerosis. The study was published in the journal Arthritis Research and Therapy and is entitled “Stress-Doppler-Echocardiography for early detection of systemic sclerosis associated pulmonary arterial hypertension.”
Systemic sclerosis is a rare, chronic autoimmune disease in which the body’s own immune system attacks healthy tissues, resulting in an abnormal growth of connective tissue and thickening of the skin. Systemic sclerosis usually affects the skin, but it can also affect internal organs such as the lungs. One of the most severe organ complications and a leading cause of death in these patients is pulmonary arterial hypertension (PAH), which is characterized by an abnormally high blood pressure in the pulmonary artery. Early detection of PAH in systemic sclerosis patients is therefore vital.
Echocardiography performed at rest is the most accurate, non-invasive method for detecting pulmonary hypertension. Studies have also reported that systemic sclerosis patients with PAH have an impaired physical exercise capacity. In the study, researchers conducted a prospective screening trial (NCT01387035) in 76 systemic sclerosis patients to determine the sensitivity and specificity of stress-Doppler echocardiography (SDE) for an early detection of pulmonary hypertension in comparison to echocardiography at rest. As a way to confirm the diagnosis, right heart catheterization (RHC) was performed in all patients both at rest and during exercise.
Researchers found that of the 76 participants, 22 patients (29%) had pulmonary hypertension confirmed through the RHC procedure, including 15 patients with PAH, 4 with left heart diseases and 3 with lung diseases. Echocardiography at rest failed in diagnosing pulmonary hypertension in 5 out of these 22 patients (cut-off value defined as systolic pulmonary arterial pressure higher than 40 mmHg), but was found to have a sensitivity of 72.7% and a specificity of 88.2% overall. In addition, SDE only failed in diagnosing pulmonary hypertension in one of the 22 patients where the cut-off value for the test was defined as systolic pulmonary arterial pressure higher than 45 mmHg during low-dose exercise, and had an improved sensitivity of 95.2%, but a reduced specificity of 84.9%.
The team concluded that SDE greatly improved the sensitivity of the detection of pulmonary hypertension in comparison to echocardiography at rest, and suggests that systemic sclerosis patients should be screened for pulmonary hypertension both at rest and during exercise.



