Lungs Affected by Idiopathic Pulmonary Fibrosis May Benefit From Inflammation
Written by |
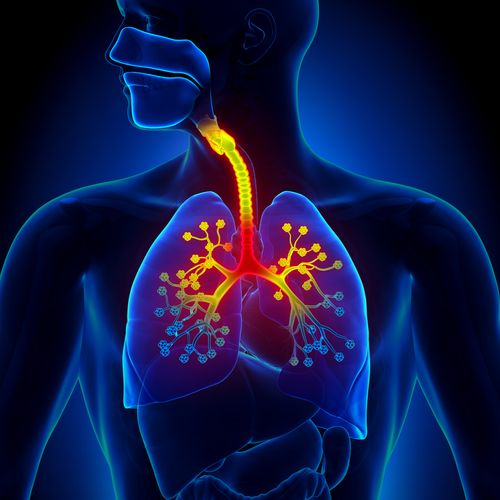
 Despite the widely held observation that inflammation leads to deadly scarring in idiopathic pulmonary fibrosis, according to a new study conducted at the National Jewish Health, some inflammation may help in the healing and repair process of the lung. Assistant professor of cell biology Elizabeth Redente, PhD, and her research team discovered that the pro-inflammatory cytokine TNF-α is able to speed recovery of damaged lungs, as well as accelerate the resolution of the disease, during their research on a mouse model.
Despite the widely held observation that inflammation leads to deadly scarring in idiopathic pulmonary fibrosis, according to a new study conducted at the National Jewish Health, some inflammation may help in the healing and repair process of the lung. Assistant professor of cell biology Elizabeth Redente, PhD, and her research team discovered that the pro-inflammatory cytokine TNF-α is able to speed recovery of damaged lungs, as well as accelerate the resolution of the disease, during their research on a mouse model.
Inflammation was thought to have been a conductor of scarring in the lungs, one of the key symptoms of IPF, for which there is currently no approved treatment. However, the researchers have remained interested in the inflammation process, since they have noted that anti-inflammatory therapies have no positive effect on the condition, leading them to suspect that inflammation may be part of the of the healing process.
[adrotate group=”4″]
“The role of inflammation in the development of scarring has been hotly debated in recent years,” explained Dr. Redente, whose results were recently published in the American Journal of Respiratory Cell and Molecular Biology. “Our findings show for the first time that TNF-α actually promotes inflammation during the resolution of established scarring. A little inflammation may actually be a good thing in the right place and time.”
During the clinical study, a group of mice were administrated TNF-α when their lungs were already damaged and had already developed scar tissue. The researchers observed that the pro-inflammatory cytokine TNF-α was able to accelerate the recovery process, while other mice who did not receive the substance, healed normally. The pro-inflammatory cytokine TNF-α reduced levels of collagen, which is the main constituent of scar tissue, and improved the flexibility of lung tissue, long before the natural process even begun.
The research team was also able to demonstrate that the mice that lacked TNF-α did not manage to heal, while the other group of mice eventually did. Due to the findings of the study, the scientists believe that TNF-α works as an inducer of white blood cell macrophages, making them transform from cells that promote fibrosis to cells that promote inflammation. The research also suggested that TNF-α was able to kill some of the pro-fibrotic macrophages.
[adrotate group=”3″]
“Physicians would welcome any therapy that could just slow down or stop the scarring process in the lungs,” stated the senior author on the study, David Riches, PhD, who is a professor and head of the program in cell biology at the National Jewish Health. “Our findings suggest that TNF-α not only slows the fibrotic process, but actually reverses established scarring in the lungs.”
The next step of the investigation is to understand TNF-α’s role in removing scar tissue and other processes, such as the removal of collagen-producing cells, the degradation and removal of collagen, and restoration of healthy lung cells, all of which are already being researched.



