Study Proves OCT Imaging Technique Useful for Managing PAH in Systemic Sclerosis Patients
Written by |
An imaging technique called optical coherence tomography (OCT) can effectively determine abnormalities in the lung vasculature of pulmonary arterial hypertension (PAH) patients with systemic sclerosis (SSc), a study shows.
The study, “Optical coherence tomography evaluation of pulmonary arterial vasculopathy in Systemic Sclerosis,” appeared in the journal Scientific Reports.
Knowledge of the mechanisms underlying PAH is limited, since most studies are performed on post-mortem tissues. But recent technological advances have allowed for intravascular imaging, which are now possible with advanced imaging techniques such as OCT.
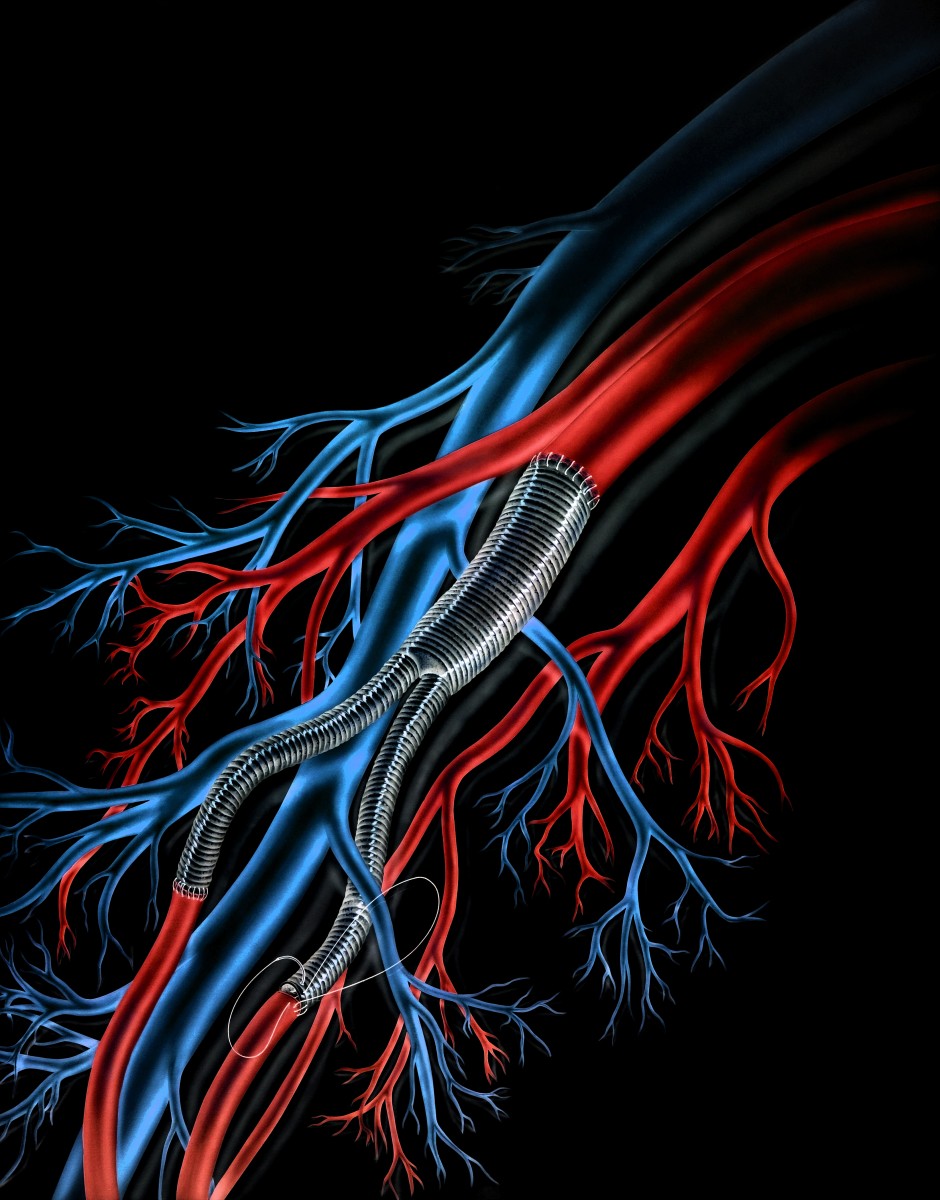
“OCT is an imaging modality analogous to ultrasound, using light instead of ultrasound, and cross-sectional images are generated using the time delay and intensity of reflected light (backscatter) from internal tissues,” researchers explained.
The technique has been successfully applied to individuals with pulmonary hypertension (PH) by finding a positive correlation between wall thickness and mean pulmonary artery pressure.
In this latest study, researchers used OCT to systematically quantify vessel wall thickness in vivo in patients with SSc-PAH. In particular, they analyzed vessels with very small diameters of less than 2 millimeters, and how these measurements correlated with blood flow parameters and response to targeted PAH treatment.
In total, researchers studied 17 SSc patients who met the criteria for PAH. They used OCT in 16 patients during right heart catheterization, a procedure performed by a surgeon using a catheter to examine the heart. The control group consisted of five patients with SSc who had no evidence on PAH upon right heart catheterization examination.
OCT analysis showed that SSc-PAH patients had significant thickening of pulmonary arteries compared to patients without PAH. This is important, because PH is known to be associated with the thickening of pulmonary arteries.
Additionally, the analysis showed, “for the first time a direct link between a structural abnormality of pulmonary arteries and a response to targeted treatment in vivo.” In fact, the team observed that SSc-PAH patients responding well to targeted PAH treatment exhibited a significantly greater number of small branches on pulmonary arteries. Researchers also found that OCT could identify the presence of blood clots and assess the potential risk of pulmonary artery thrombus formation.
Overall, the results support the use of OCT as a measure to evaluate changes in pulmonary vasculature in patients with SSc-PAH, to assess treatment response, and to identify patients who could benefit from anticoagulation treatment.



