In PAH, Tissue Phase Mapping of Left Ventricle May Predict Clinical Outcomes
Written by |
In a new study, researchers used novel cardiovascular magnetic resonance (CMR) tissue phase mapping (TPM) to determine if right ventricular disease in pulmonary hypertension (PH) patients also resulted in abnormal left ventricular functioning, discovering that left ventricular myocardial velocities are significantly abnormal in PH and also constitute independent predictors of clinical outcome.
The research paper, “Left ventricular diastolic dysfunction in pulmonary hypertension predicts functional capacity and clinical worsening: a tissue phase mapping study,” was published in the Journal of Cardiovascular Magnetic Resonance.
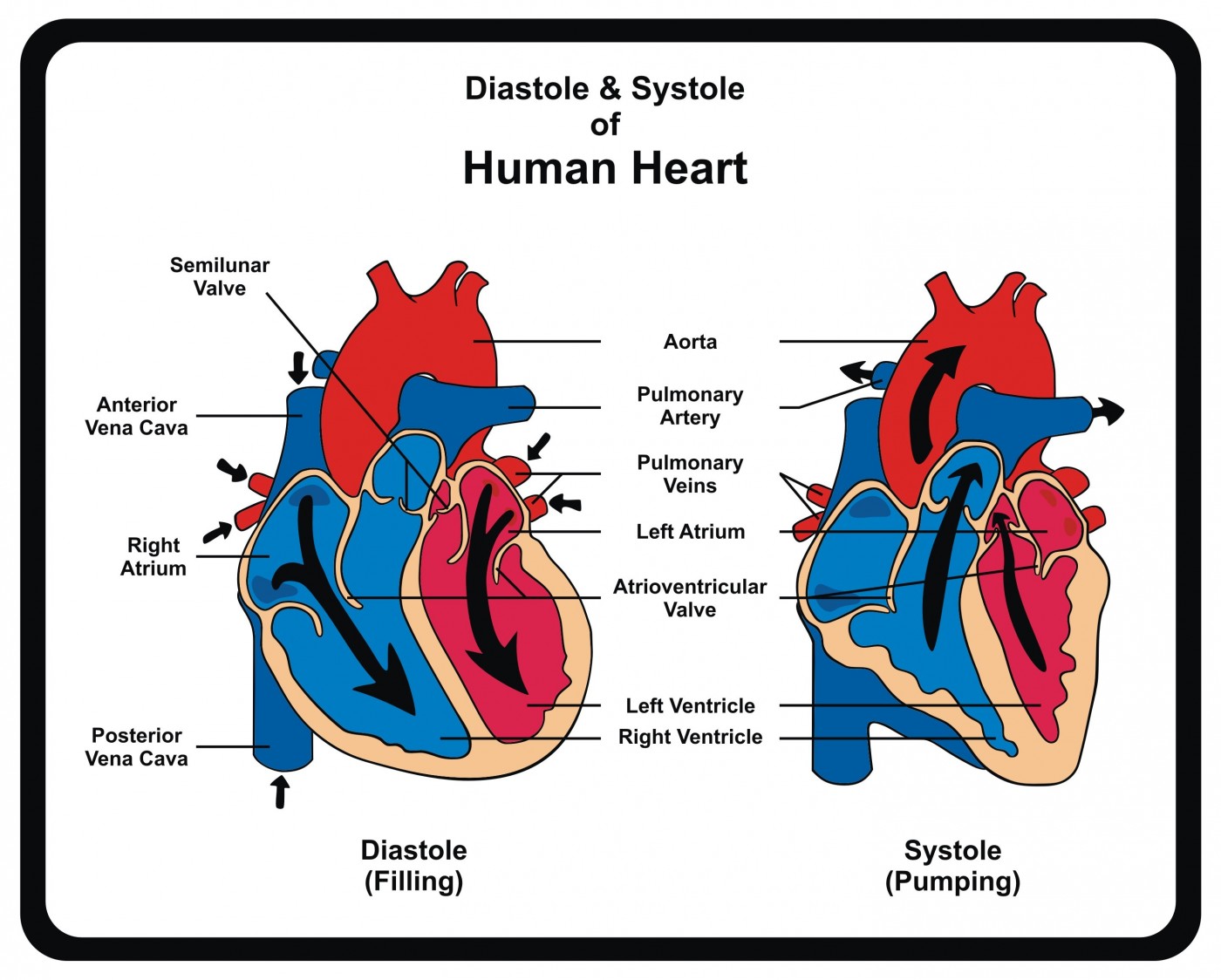
Pulmonary hypertension (PH) is a life-threatening disease characterized by high blood pressure, increased pulmonary artery pressure, and right ventricular (RV) dysfunction and failure. Cardiovascular magnetic resonance (CMR), the standard diagnostic method of assessing RV function, is routinely used in PH. Several studies have shown that assessment of RV volumes and ejection fraction (EF) is useful for PH prognosis. Although left ventricular ejection fraction (LVEF) has been shown to be reduced in late stage PH, most PH patients have normal LVEF. However, researchers theorize that, due to ventricular interdependence, it is likely that these patients have some kind of LV dysfunction and if so assessment of LV myocardial mechanics may be clinically relevant.
The scientists used tissue phase mapping (TPM) to assess radial, longitudinal, and tangential myocardial velocities in 40 patients with PH and 20 healthy matched volunteers. Main results showed that patients with PH had reduced global E rad and E long velocities, peak global E rad velocity was an independent predictor of 6 minute walking distance (6MWD), and peak global E long velocity was an independent predictor of clinical worsening.
Researchers concluded that “TPM metrics of LV diastolic dysfunction in PH reliably discriminate between health and disease, and are also strongly predictive of functional capacity. TPM may also be incrementally beneficial in identifying clinical worsening in PH compared with conventional CMR metrics of RV function. These feasibility data support the application of the technique to a larger group of patients over a longer follow-up period. This would allow full determination of the prognostic capacity of LV TPM metrics in PH.”



