Researchers Determine eRAP As Viable PAH Prognosticator
Written by |
 A new study on pulmonary arterial hypertension (PAH) entitled “Echocardiographic Assessment of Estimated Right Atrial Pressure and Size Predicts Mortality in Pulmonary Arterial Hypertension” was published in Chest by Dr. Christopher Austin, part of Dr. Brian Shapiro’s group from Division of Cardiovascular Disease at the Mayo Clinic, showing that estimated right atrial pressure (eRAP), measured by echocardiography, may be an effective prognostic indicator in patients with pulmonary arterial hypertension (PAH).
A new study on pulmonary arterial hypertension (PAH) entitled “Echocardiographic Assessment of Estimated Right Atrial Pressure and Size Predicts Mortality in Pulmonary Arterial Hypertension” was published in Chest by Dr. Christopher Austin, part of Dr. Brian Shapiro’s group from Division of Cardiovascular Disease at the Mayo Clinic, showing that estimated right atrial pressure (eRAP), measured by echocardiography, may be an effective prognostic indicator in patients with pulmonary arterial hypertension (PAH).
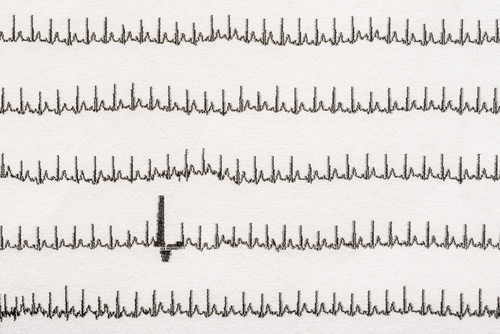
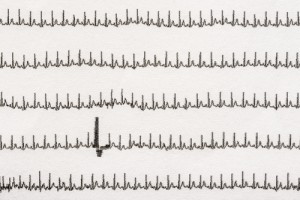
Pulmonary arterial hypertension (PAH) occurrence continues to increase, and is a clinical problem concerning the recognition and management of patients. This heterogeneous pathological condition continues to show a significant morbidity and mortality rates. Elevated mean right atrial pressure (RAP) measured by cardiac catheterization is an independent risk factor for mortality. Previous studies have shown a modest association with invasive and noninvasive echocardiographic right atrial pressure (eRAP), but the prognostic relevance of eRAP has not been previously addressed in PAH patients. Echocardiography is considered a crucial screening technique for estimating the right ventricular systolic pressure (RVSP) and assessment of right ventricular size and function.
[adrotate group=”4″]
Dr. Brian Shapiro and co-authors made a retrospective analysis of 121 patients with PAH and found that an elevated eRAP correlated significantly with reduced transplant-free survival. High eRAP was defined as greater than 15 mmHg, according to the American Society of Echocardiography (ASE) 2005 guidelines. The probability of death or transplant was increased 7.94-fold and 2.61-fold for patients with elevated eRAP according, respectively, to the 2005 ASE definition (>15 vs ≤5 mmHg) and to the 2010 definition (high vs normal). But in multivariate analysis, only the 2005 definition was associated with death or transplant, at a 2.28-fold increased risk. During the 3 years of follow-up, transplant-free survival ranged from 82% for patients with low eRAP to 13% for those with high eRAP.
The research team addressed the prognostic value of right atrial area (RAA) “since eRAP may be technically prohibitive in some patients,” said the researchers.
[adrotate group=”3″]
Patients with an enlarged RAA (>18 cm2) had a transplant-free survival rate of 50% when compared with 76% for those with a normal RAA, equating to a 2.56-fold increased risk among those with an enlarged RAA. However, on a multivariate analysis this difference was not significant.
The researchers highlighted that eRAP is an “inexpensive and easily obtained predictive measure” in PAH patients and concluded that it should be “an essential component of the right heart evaluation.”



