Smooth Muscle and Other Cells Send Signals That Promote PH Progression, Early Study Finds
Written by |
Signaling, or “crosstalk,” between smooth muscle and other cells in the lungs’ vasculature can promote the progression of pulmonary hypertension, research in mice shows. The findings point to mechanisms underlying PH that may lead to new treatments, especially ones targeting early stages of the disease.
The research “Cell Autonomous and Non-cell Autonomous Regulation of SMC Progenitors in Pulmonary Hypertension” was published in the journal Cell Reports. Its authors call for more studies into such signaling as it may have “major ramifications” for treatment development.
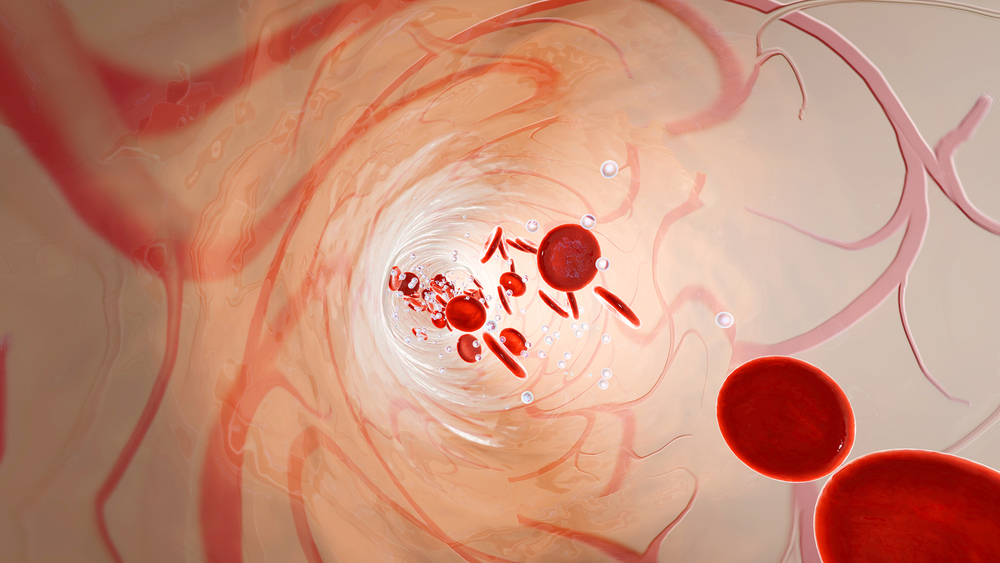
PH is marked by increased pulmonary arterial pressure and hyper-muscularization of the lung vasculature. Throughout its course, smooth muscle cells (SMCs) — which form a sheath around bronchi and blood vessels in the lungs — go through marked changes. But what signals, or crosstalk, leads specialized cells to proliferate and migrate within vessels of the lung remains poorly understood.
Scientists at the Yale Cardiovascular Research Center investigated molecular signals that may be shared between SMCs and other cells present in the lung’s blood vessels of a PH mouse model. By looking at such signaling, the study focused on vasculature changes in earlier disease phases.
They found two signals, called KLF4 and HIF1-alpha, that play a direct role in SMCs and promoted PH progression within a context of low oxygen or hypoxia — hypoxia being a major cause of PH.
Specifically, the transcription factor KLF4 is critical for initiating the distal (distant) migration of smooth muscle cells in PH; HIF1-alpha is key for the subsequent steps of pulmonary arteriole muscularization.
In addition, researchers found that signals from other cells in the lung vasculature, namely endothelial cells and macrophages (cells of the immune system), also contribute to SMC multiplication and migration — the two steps that lead to the narrowing and blockage of lung blood vessels that characterize this disease.
“The interplay among distinct cell types is critical for the pathogenesis of diverse vasculoproliferative diseases but generally is understudied and poorly understood,” the researchers wrote.
“Thus, pathological studies delineating intercellular mechanisms — such as this investigation of specialized SMC progenitors in PH — are needed, because the resulting insights promise to have major ramifications for the development of novel therapeutic strategies,” the team concluded.