Treating Inflammation in PAH Using Antioxidant Inflammation Modulators

 Pulmonary Arterial Hypertension (PAH) is a life-threatening disease in which endothelial dysfunction, vasoconstriction in small pulmonary arteries, dysregulated proliferation of vascular cells, and dysregulated inflammatory signaling leads to pulmonary arterial obstruction increasing pulmonary vascular resistance and resulting in right ventricular failure.
Pulmonary Arterial Hypertension (PAH) is a life-threatening disease in which endothelial dysfunction, vasoconstriction in small pulmonary arteries, dysregulated proliferation of vascular cells, and dysregulated inflammatory signaling leads to pulmonary arterial obstruction increasing pulmonary vascular resistance and resulting in right ventricular failure.
Different types of treatments for PAH exist that can improve patients’ symptoms through vasoconstriction relief, such as prostanoids, endothelin receptor antagonists, phosphodiesterase 5 inhibitors, soluble guanylate cyclase stimulants or, rarely, certain calcium channel blockers. However useful, these treatments do not directly suppress inflammation or proliferation pathways involved in the disease, allowing it to progress.
With the eminent clinical need for a new PAH therapy, an extensive body of leading academic scientists has been developing cutting edge investigations for production of novel drugs. Among those developing therapies for the disease, Reata Pharmaceuticals, Inc. is developing a novel class of drugs with potent transcriptional activity called antioxidant inflammation modulators (AIMs). The company has already focused early research collaborations involving the therapeutic use of AIMs in treating several diseases such as melanoma, lung cancer, Freidreich’s Ataxia, Mitochondrial Myopathies, and Radiation Dermatitis, as well as for RTA402 (also known an bardoxolone methyl), an AIM being tested and developed as a potential therapy for treating the underlying inflammation in PAH.
[adrotate group=”4″]
Getting To Know AIMs
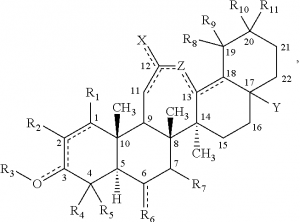
Several studies have demonstrated that AIMs can affect the activity of major transcription factors, leading to complex downstream effects that influence the expression of hundreds of genes. These modulators derive from oleanolic acid, a naturally occurring triterpenoid found in food and medicinal plants, and bind to key regulatory cysteine residues on Keap-1, a protein that is the main negative regulator of the transcription factor NrF2. Once NrF2 is activated, is translocates to the cellular nucleus and stimulates the production of a wide variety of proteins with antioxidative, anti-inflammatory, and cytoprotective properties. Furthermore, activated Nrf2 reduces the production of reactive oxygen and nitrogen species (ROS/RNS), such as superoxide, hydrogen peroxide, and peroxynitrite, and inhibit the activity of the major pro-inflammatory transcription factor NF-kB, either directly by inhibiting IKKβ, the kinase that activates NF-kB, or indirectly through inhibition of ROS/RNS-mediated signaling pathways that promote NF-kB activity. Such pharmacological activity simulates that of endogenous prostaglandin metabolites responsible for the resolution of inflammation. As such, AIMs can inhibit inflammatory cytokine signaling including TNFa, IL-6, IL-1, IFN-g and IL-17; they can inhibit ROS/RNS-mediated effects of excessive inflammatory response, such as inhibition of nitric oxide production by activated macrophages; they can inhibit proliferative signaling pathways, like that observed in cancer cell replication in vitro and in vivo; and they can reduce the production of enzymes associated with tissue remodeling, such as MMP9 and MMP2 proteases that are associated in the progression of cancer, arthritis and several other diseases.
With such a direct effect on different immune-related molecules, the impact AIMS could have on patients suffering from immune disorders will be an important clinical focus. “I am particularly interested if bardoxolone will show a greater effect in subsets of patients such as HIV and other related PAH diseases,” Harrison W. Farber, M.D. Professor of Medicine and Director of the Pulmonary Hypertension Center, Boston University, Boston Medical Center, told Pulmonary Hypertension News in an exclusive interview.
[adrotate group=”3″]
In addition to the anti-inflammatory effects, AIMs have also been shown to hold strong cytoprotective effects. They are able to reduce the expression of iNOS, an enzyme involved in immune responses, and increase the expression of glutathione, thioredoxin reductase and superoxide dismutase, key antioxidative peptides and proteins. Moreover, AIMs have been demonstrated to reduce the formation of markers of DNA damage in a model of aflatoxin-induced liver cancer, a chemically induced model of Parkinson’s disease and in cells exposed to high-dose radiation.
Due to the role Nrf2 plays in transcriptionally regulating multiple genes involved in the production of cellular energy, AIMs can broadly activate intracellular and mitochondrial anti-oxidative pathways. In fact, animal model studies have proven that AIMs increase oxygen consumption, reduce insulin resistance and improve glucose clearance in animal models of diet-induced obesity and diabetes, leading to the development of clinical trials where bardoxolone methyl showed positive effects on glucose clearance and weight loss in patients with Type II diabetes.
 Bardoxolone Methyl, PAH & Beyond
Bardoxolone Methyl, PAH & Beyond
Because AIMs can target such a broad spectrum of biological processes, they can have promising effects in targeting not only PAH but also several different diseases that have as commons grounds exacerbated inflammatory processes. One such disease is radiation dermatitis, a condition whereby patients receiving radiation therapy for different types of cancer develop dose-dependent skin damage as a result from radiation-produced oxidative stress. Since AIMs are potent inducers of antioxidative systems, they can protect normal tissues against this damage. As such, in mouse models of radiation dermatitis and radiation-induced mucositis, AIMs have shown highly significant protective activity, reducing the peak intensity and duration of injury.
Of extreme relevance is the capacity of these small modulating molecules to inhibit the induction of antigen-specific T cell tolerance by tumor cells, making them potential candidates for tumor immunotherapy. Even though cancer is not an inflammatory disease per se, tumor progression is dependent on an inflammatory microenvironment, where various inflammatory cells inhabit and a network of signaling molecules is indispensable for the malignant progression of transformed cells, involving the activation of NF- κB and Nrf2, both direct targets of bardoxolone methyl.
Data from published studies has shown that AIMs were able to inhibit the production of ROS/RNS by myeloid-derived suppressor cells, therefore allowing T-cell recognition of tumor cells. Also, AIM treatment was shown to improve immune cell infiltration of tumors and enhance the anti-tumor effects of a cancer vaccine, while promoting the maturation of dendritic cells, a type of cell essential for presentation of antigens to the immune system. Furthermore, AIMs have been documented to induce apoptosis of tumor cells, inhibit metastasis, increase the efficiency of chemotherapy and radiation therapy, and prevent early tumor formation and growth.
By targeting PAH beyond basal dilation and decreasing cell proliferation, bardoxolone methyl could benefit PAH patients in a way that currently available therapies are not capable of. “If Bardoxolone works in PAH without untoward effects on the immune system, then potentially it will be disease changing and not another vasodilator,” Dr. Farber explained.
Based on the growing scientific evidence, bardoxolone methyl may act as a promising antioxidant inflammation modulator to treat not only PAH but also a multitude of other serious conditions.