CTEPH Found To Be Underdiagnosed; Survey Reveals Need for Greater Physician Awareness
Written by |
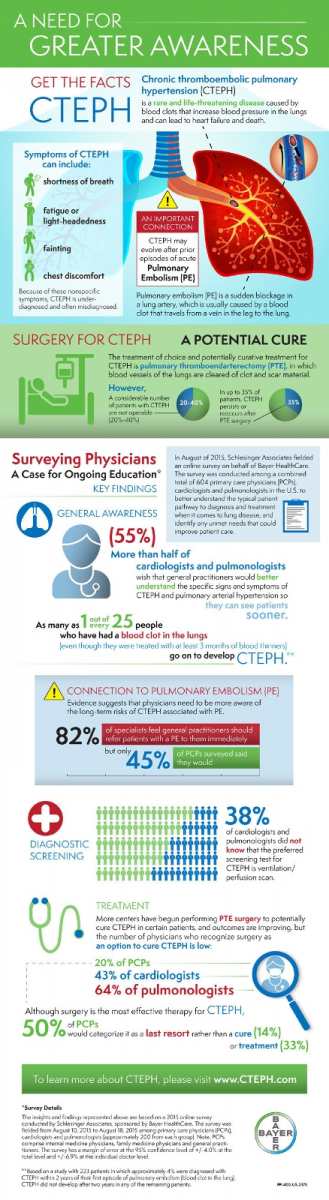
A new survey sponsored by Bayer has revealed that many physicians report a lack of familiarity with a condition called chronic thromboembolic pulmonary hypertension (CTEPH). The 2015 Bayer PH Physician Survey was released on November 24 to help draw attention to CTEPH and the need for stepped-up education efforts to improve the patient pathway to diagnosis and effective treatment of the disorder.
CTEPH is a rare, life-threatening form of pulmonary hypertension (PH) — the result of multiple or recurrent blood clots in the lung, also known as pulmonary embolism (PE). In CTEPH, a thrombus (clot-like mass) gets stuck to the lungs blood vessel wall and blocks blood flow, with the clot(s) and resulting scar tissue limiting the blood supply to the arteries in the lungs, leading to PH, strain and eventually failure of the right side of the heart.
Bayer notes that while all five types of PH share certain common characteristics, there are differences that occur with CTEPH, distinguishing it from other forms of PH, such as the more commonly known pulmonary arterial hypertension (PAH). The most common CTEPH symptoms are similar to those that characterize PH, including shortness of breath with exercise, fatigue, or weakness. While CTEPH can be life-threatening, it is the only type of PH that can be cured in some people with a type of surgery called PTE, or pulmonary thromboendarterectomy.
Bayer’s CTEPH.com site estimates that about 600,000 people in the US have an acute pulmonary embolism, with between 500 and 2,500 new CTEPH cases diagnosed annually, referencing a study entitled “Incidence and prevalence of chronic thromboembolic pulmonary hypertension: from acute to chronic pulmonary embolism” (Proc Am Thorac Soc. 2006;3:564-7) by Tapson V et al. However, Bayer notes that CTEPH’s incidence and prevalence are yet to be precisely determined, and these estimates may be significantly on the low side. It’s also noted that based on a study with 223 patients in which approximately four percent were diagnosed with CTEPH within two years of their first episode of pulmonary embolism, as many as one out of every 25 people who had a pulmonary embolism (even if they were treated with at least three months of anticoagulants) go on to develop CTEPH.
CTEPH risk factors include having experienced an acute pulmonary embolism (PE) — a blood clot in the lungs that can develop when a certain type of blood clot called deep vein thrombosis (DVT) travels from the leg or another part of the body to an artery in the lung, where it gets stuck. An acute PE can cause shortness of breath, chest pain, and coughing up blood, and while CTEPH is rare, it generally appears in someone within six months to two years of experiencing an acute PE, and especially in persons who have experienced more than one PE in their lifetime.
Unfortunately, there is no way to determine whether a patient definitely has CTEPH based on symptoms alone, due to the most common symptoms of CTEPH — shortness of breath, fatigue, light-headedness, fainting and chest discomfort — also being common symptoms associated with other diseases, such as asthma, chronic obstructive pulmonary disease (COPD), heart failure, or acute PE.
Besides experiencing an acute PE, other conditions that can cause CTEPH include spleen removal, having infected surgical cardiac shunts, pacemakers or defibrillator leads, chronic inflammatory disorders, thyroid replacement therapy, cancer, and having a high risk for blood clots, although Bayer adds that it is possible to develop CTEPH without a history of an acute PE or any of the above-cited conditions.
CTEPH treatment includes anticoagulants — drugs commonly called blood thinner — which can help prevent clots from forming in the bloodstream.
CTEPH is also potentially curable with a type of surgery called pulmonary thromboendarterectomy (PTE), in which blood vessels of the lungs are cleared of clot and scar material, and which is the recommended treatment for CTEPH for eligible individuals, although not everyone qualifies. Patients with pulmonary artery blockages that cannot be reached by the surgeon and are therefore inoperable are not PTE candidates. However even after PTE surgery, CTEPH symptoms may persist, with several studies finding that CTEPH relapsed in approximately 1 out of 10 people who underwent the CTEPH procedure — a subset of the disease known as recurrent CTEPH.
Need For Greater CTEPH Awareness
 “Because surgery can be an effective treatment for CTEPH, it is critical that physicians suspect and diagnose the condition. Unfortunately, as demonstrated by this survey, recognition of CTEPH among primary care physicians is inadequate,” says Richard Channick, M.D., director of Massachusetts General Hospital’s Pulmonary Hypertension and Thromboendarterectomy Program in a Bayer release. “We very much need further education to identify and treat these patients as quickly as possible.”
“Because surgery can be an effective treatment for CTEPH, it is critical that physicians suspect and diagnose the condition. Unfortunately, as demonstrated by this survey, recognition of CTEPH among primary care physicians is inadequate,” says Richard Channick, M.D., director of Massachusetts General Hospital’s Pulmonary Hypertension and Thromboendarterectomy Program in a Bayer release. “We very much need further education to identify and treat these patients as quickly as possible.”
The Bayer-sponsored survey of 604 PCPs, cardiologists and pulmonologists (approximately 200 from each group — 202 PCPs, 202 cardiologists and 200 pulmonologists) was conducted online by Schlesinger Associates from August 10, 2015 to August 18, 2015. For the survey, internal medicine physicians, family medicine physicians and general practitioners were considered PCPs. The survey has a margin of error at the 95 percent confidence level of +/-4.0 percent at the total level and +/-6.9 percent at the individual doctor level.
Additional findings of the survey illustrate that:
• Additional education on the preferred diagnostic test to identify CTEPH is needed because its nonspecific symptom profile means the disorder is underdiagnosed and often misdiagnosed. A ventilation/perfusion (VQ) scan is the preferred test for screening for chronic thromboembolic disease, and should be viewed as an initial step in the diagnosis of CTEPH (Simonneau G, et al. J Am Coll Cardiol. 2009;54(suppl 1):S43-S54) but 38 percent of cardiologists and pulmonologists surveyed were not aware of that guideline.
• The researchers found substantial under-recognition of PTE surgery as a potential cure for CTEPH, although the survey did find that more medical centers have begun performing PTE surgeries, and outcomes are improving. Nevertheless, the number of physicians who recognize PTE as an option to cure CTEPH remains low 20 percent of PCPs, 43 percent of cardiologists and 64 percent of pulmonologists, and while surgery is the most effective therapy for CTEPH (Piazza G and Goldhaber SZ. N Engl J Med. 2011;364:351-360 ), 50 percent of PCPs would categorize it as a last resort, rather than a cure (14 percent) or treatment (33 percent).
• There is lack of awareness of the connection between pulmonary embolism and CTEPH, and diagnosis of CTEPH — which is critical, as it is a potentially curable form of PH — requires an appropriate diagnostic workup. As many as 1 out of every 25 previously treated patients with PE could develop CTEPH (Tapson V et al. ibid), but according to the survey results, while 82 percent of specialists think general practitioners should refer patients with a PE to them immediately, only 45 percent of PCPs surveyed said they would. Specialists wish PCPs would refer patients with lung disease symptoms, including those of CTEPH, to them sooner, and more than half (55 percent) of cardiologists and pulmonologists surveyed wish that general practitioners would better understand the specific signs and symptoms of CTEPH and pulmonary arterial hypertension (PAH), so that they can see patients sooner.
“Together with treating physicians, our goal is always to find ways to raise awareness about this misunderstood disease,” says Dario Mirski, M.D., vice president and head, U.S. medical affairs at Bayer. “For patients with CTEPH, the benefits of surgery may be very positive, and we hope the results of this survey help drive conversations about optimal diagnostic tools and treatment among physicians and the patient community.”
Some practical lifestyle and dietary tips about living with CTEPH can be found at:
https://www.cteph.com/living-with-cteph/diet-and-exercise/
For more information, go to:
https://www.cteph.com
and
https://www.bayer.com
Sources:
Bayer HealthCare
CTEPH.com
The Pulmonary Hypertension Association of Canada
Infographic Courtesy Bayer HealthCare