Pulmonary Hypertension Reversed with Mitochondrial Transplant in Rats
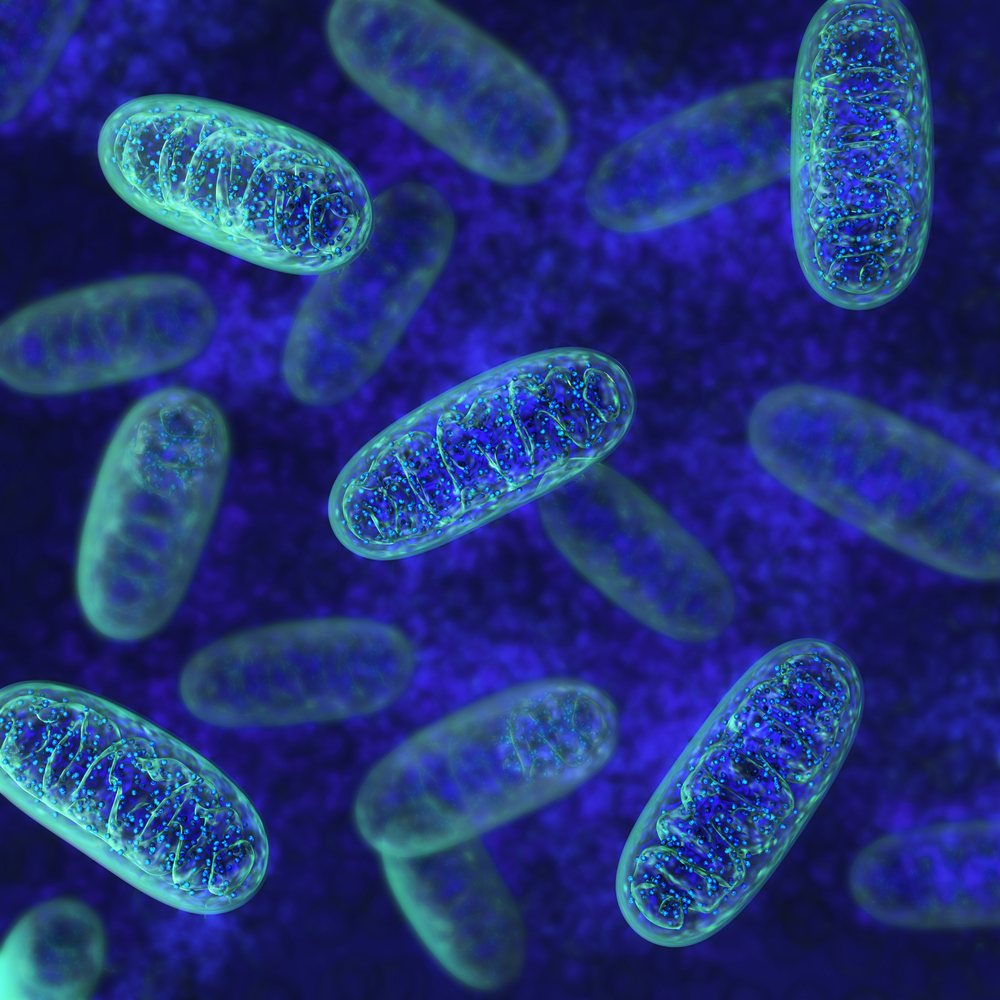
Mitochondria in lung arteries responds in an opposite way to a lack of oxygen compared to mitochondria in other parts of the body, as they constrict and remodel blood vessels. This finding allowed researchers to reverse pulmonary hypertension in rats by transplanting mitochondria from a leg artery to the lung by simply injecting them into the bloodstream.
The findings were published in the journal Oncotarget in a report titled “Mitochondrial transplantation attenuates hypoxic pulmonary hypertension,” and indicate that although human tests of such mitochondrial transplants are still in the future, studies will eventually reveal if mitochondria might be a good target in the development of new treatments for pulmonary hypertension.
Earlier research gave scientists at the Huazhong University of Science and Technology in China hints that mitochondria, known as our cellular powerhouses, might be involved in lung changes following hypoxia (low oxygen levels). Low oxygen is a known trigger for pulmonary hypertension, resulting from the constriction and remodeling of blood vessels in the lung.
In previous experiments, the research team had shown that when exposed to hypoxia, lung mitochondria contributed to these processes, causing constriction and vessel remodeling. This was, however, a feature not shared by mitochondria in the legs or other body parts, which instead helped blood vessels to relax in low-oxygen conditions.
The research team figured that these differences might be used to treat pulmonary hypertension. So, they isolated the cellular components from a large artery in the leg of rats living in low-oxygen conditions, and injected them intravenously into other hypoxic rats that had already started developing pulmonary hypertension. The transplanted cell parts were labeled with a fluorescent dye, allowing researchers to keep track of their movements.
After several hours, the mitochondria could be found in the endothelial cells lining the lung blood vessels, and soon after they appeared in blood vessel’s smooth muscle cells. Once the leg mitochondria had entered the lung vessels, they prevented the constriction and vascular remodeling of the arteries observed in rats also exposed to brief periods of hypoxia.
The mitochondrial transplant could also prevent pulmonary hypertension when transplanted to rats before hypoxia exposure, and reverse already established disease in rats living several weeks in low-oxygen cages, suggesting that transplanting mitochondria from another body part of a patient might be a way to treat the disease.
Before human studies can take place, however, any potential long-term side effects of such a treatment need to be studied in detail.