In Certain CTEPH Patients, Vascular Remodeling May Lead to Hypoxemia
Patients with chronic thromboembolic pulmonary hypertension (CTEPH) who are successfully treated with pulmonary endarterectomy (PEA) may be at increased risk of having low levels of oxygen in the blood due to severe pulmonary arteriopathy, a condition characterized by pulmonary artery remodeling, according to a study from Chiba University in Japan.
The study, “Severe Pulmonary Arteriopathy Is Associated with Persistent Hypoxemia after Pulmonary Endarterectomy in Chronic Thromboembolic Pulmonary Hypertension,” published in the journal PLOS One, suggests that reversing pulmonary artery remodeling may improve both hypoxemia and residual pulmonary hypertension (PH) in these patients.
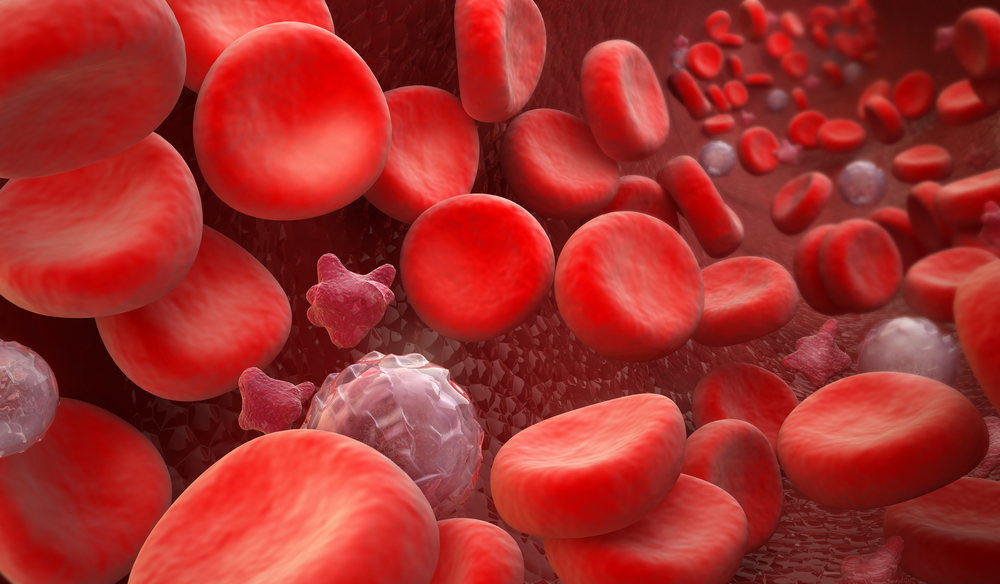
CTEPH is a form of pulmonary hypertension characterized by occlusion of pulmonary arteries by chronic blood clots, which are thought to emerge from inappropriate resolution of acute pulmonary embolism.
PEA, a surgical procedure that removes the organized pulmonary blood clots, has been shown to improve the condition of CTEPH patients, showing benefits in blood flow, cardiac function, and the six-minute walk distance test.
However, following PEA, many patients exhibit persistent hypoxemia (low levels of oxygen in the blood) and residual PH, both of which are associated with poor functional capacity. In fact, 50 to 60 percent of CTEPH patients experience persistent hypoxemia following successful PEA.
Recently, researchers showed that residual PH was associated with severe pulmonary arteriopathy, which led them to hypothesize that these modifications in pulmonary arteries could be involved in impaired oxygen exchange.
Now, researchers examined 23 CTEPH patients who underwent PEA and lung biopsy between December 2011 and November 2014. The team quantified the extent of pulmonary arteriopathy through lung biopsies and analyzed the relationship between gas exchange and the severity of pulmonary remodeling after PEA.
Results revealed that oxygen levels negatively correlated with the extent of pulmonary artery remodeling after PEA, but not before PEA. In addition, a multivariate analysis showed that the obstruction ratio and patient age were determinants to the oxygen levels one month after PEA.
Similarly, obstruction ratio and improvement of pulmonary vascular resistance were determinants of oxygen levels at follow-up, which was performed on average 13 months after PEA.
“Removal of chronic segmental pulmonary thrombi by PEA would be expected to increase blood flow to distal vascular areas, but persistent pulmonary arteriopathy would cause a chronic disruption of blood flow into the pulmonary capillary bed,” the researchers wrote in their report.
Low blood oxygen levels may be caused by several mechanisms, including a mismatch in the lung areas that are highly perfused with blood with those that receive high amounts of air; impaired gas exchange; and hypoventilation, characterized by reduced amounts of air entering the lung alveoli.
The team believes that the hypoxemia observed in these CTEPH patients is a result of ventilation-perfusion mismatch and impaired oxygen diffusion, caused by pulmonary artery remodeling. Importantly, they believe that treating patients with pulmonary vasodilators may improve their outcomes, but it remains to be addressed which vasodilators have beneficial effects on these CTEPH patients.