S1P Molecule Seen to Promote PAH, May Offer New Way of Treating Disease
Written by |
Patients with pulmonary arterial hypertension (PAH) have higher than usual blood levels of S1P, a molecule that promotes worsening disease, according to a study published in the journal Pulmonary Circulation. The researchers, working in a rat PAH model, also found that blocking this protein improved pulmonary arterial structure and cardiac function, suggesting that drugs targeting S1P may be potential PAH therapies.
The study, “Sphingosine-1-Phosphate Is Involved In The Occlusive Arteriopathy Of Pulmonary Arterial Hypertension,” was conducted by a research team at the College of Medicine, University of South Alabama.
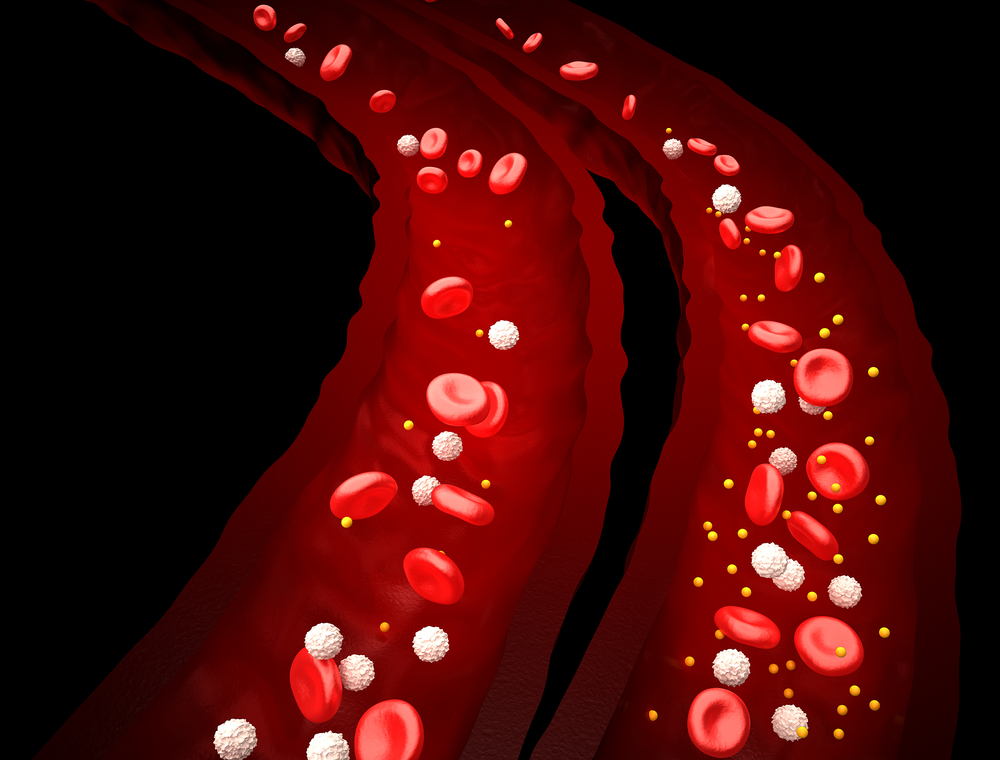
S1P is a lipid (fat) produced by proteins SphK1 and 2, and is known to regulate several processes involved in the development of PAH, including vasoconstriction (tightening of the blood vessels), inflammation, and fibrosis.
To examine whether S1P contributed to PAH, researchers used blood and lung tissue samples from patients with idiopathic PAH (IPAH) and healthy subjects, as well as from rats with PAH. They observed that the expression levels of S1P were increased in both the PAH patients and rats, and that levels of both SphK1 and SphK2 rose in step with disease progression (and further increased the production of S1P).
Using rat cultures of pulmonary arterial endothelial cells (cells of the arterial walls), the team observed that increased S1P production promoted cell proliferation. They then treated the PAH rats with an SphK1 inhibitor (SLP7111228) for three weeks, and saw that treatment reduced both S1P levels in the blood and lesions in the artery walls, one of the hallmarks of severe PAH. The treatment also improved cardiac function and pulmonary artery resistance, both of which are affected in PAH. The inhibitor was not able to reduce blood pressure in the right heart ventricle or its hypertrophy, but the researchers suggested that treatment for longer periods may improve these as well.
“[W]e found that circulating levels of S1P were elevated in patients with IPAH and in a rat model of severe occlusive PAH,” the authors wrote. “Importantly, inhibition of S1P synthesis improved the pulmonary arterial structure and cardiac function of the PAH rats. We further identified S1P as a proliferative mediator of rat [pulmonary artery cells].”
They concluded, “Our study supports that S1P is involved in the pathogenesis of occlusive arteriopathy in PAH and provides further evidence that S1P signaling may be a novel therapeutic target.”
Current therapies can improve PAH symptoms but do not provide a cure.



