Balloon Pulmonary Angioplasty May Be ‘Important Therapeutic Option’ in CTEPH Patients, Study Suggests
Written by |
Patients with blood clots in the lungs known as chronic thromboembolic pulmonary hypertension (CTEPH) can benefit from balloon pulmonary angioplasty (BPA), a new study shows. The procedure is an alternative to the standard treatment for CTEPH — pulmonary endarterectomy (PEA) — in patients who are not eligible for PEA.
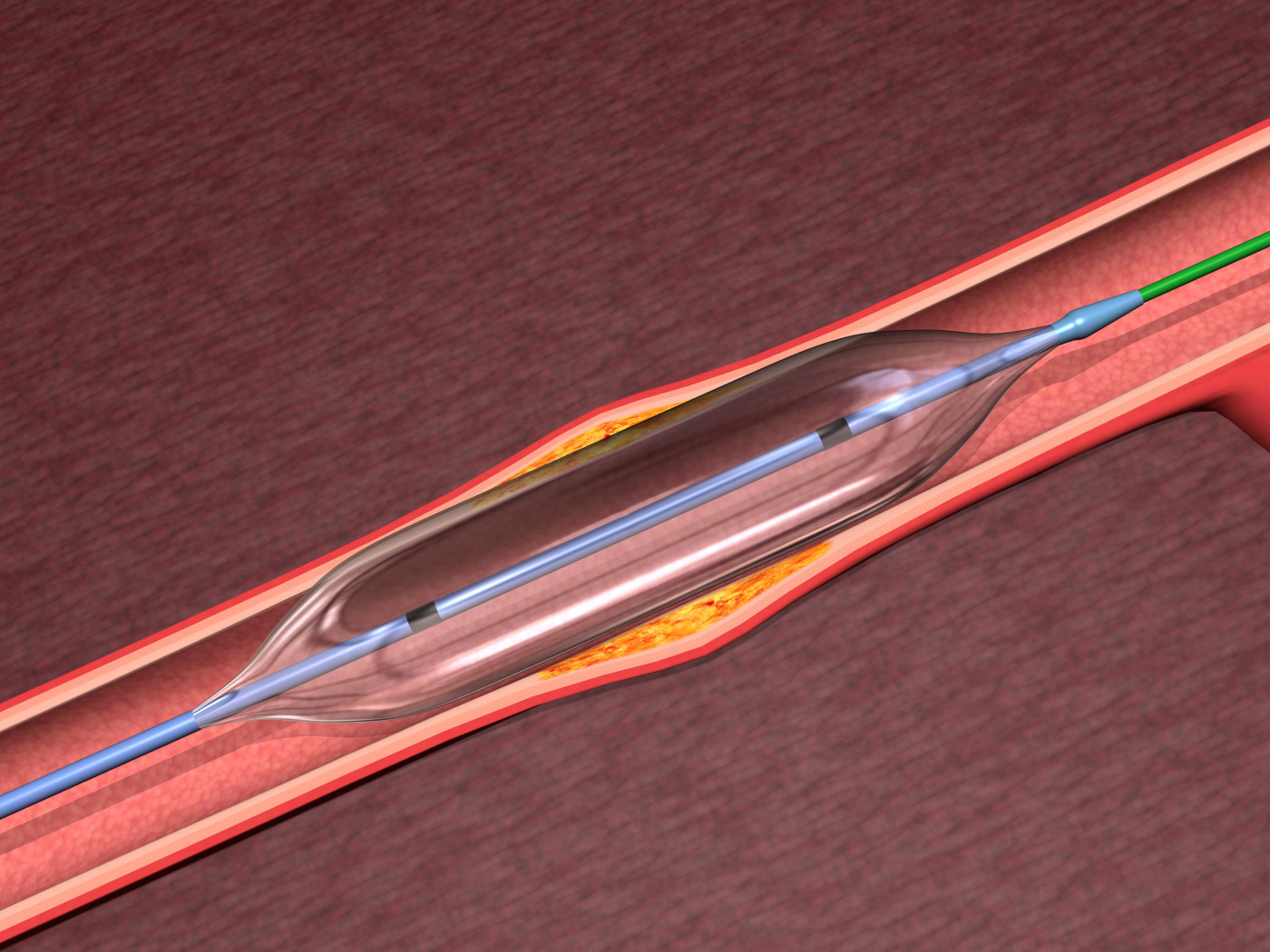
PEA involves surgery to remove blood clots in lung arteries; whereas BPA uses a very fine wire inserted into the blood vessels in the lungs that are blocked. The wire positions a balloon that is subsequently inflated for a few seconds to push the blockage aside and restore blood flow.
The findings were reported in the study titled “Balloon Pulmonary Angioplasty for Chronic Thromboembolic Pulmonary Hypertension, Results of a Multicenter Registry,” published in the journal Circulation: Cardiovascular Quality and Outcomes.
Researchers collected and analyzed data from 308 patients (62 men and 246 women, with a mean age of 61 years) who underwent 1,408 procedures at seven institutions in Japan.
Blood pressure and blood flow were found to have improved significantly in 249 patients who underwent BPA. In most cases, the procedure was terminated in those patients because of improvement in mean pulmonary arterial pressure (average blood pressure in lung arteries) or improvement in symptoms.
Improvements of hemodynamic parameters (measures of blood flow) were maintained in 196 patients who underwent right heart catheterization during the follow-up period (to measure blood pressure in the heart and lungs).
Want to learn more about the latest research in Pulmonary Hypertension? Ask your questions in our research forum.
The mean pulmonary arterial pressure dropped from 43.2 to 24.6 mm Hg after the last BPA procedure, and to 22.5 mm Hg at follow-up. The need for oxygen supplementation and PH-targeted therapies also decreased. World Health Organization functional class and exercise tolerance improved in these patients at the end of the BPA procedures.
The researchers note that overall survival rates after BPA are similar to the standard PEA treatment. Overall survival after the initial BPA procedure was 96.8% at 1 and 2 years. At 3 years, it was 94.5%.
There were complications after 511 (36.3%) BPA procedures. Injury to the lungs occurred in 17.8%. Hemoptysis (coughing up blood or bloody sputum) occurred in 14.0%, and pulmonary artery perforation occurred in 2.9% of the BPA procedures.
There were 12 deaths during follow-up. Of these patients, eight died within 30 days after BPA. The leading causes of death were multiorgan failure, right heart failure, and sepsis (blood infection).
“This multicenter registry suggested improved hemodynamic results after BPA. Complication rates were high, but overall survival was comparable with pulmonary endarterectomy. BPA may be an important therapeutic option in patients with chronic thromboembolic pulmonary hypertension,” the team concluded.



