Exosomes from Stem Cells May Slow Vascular Remodeling in PAH
Small vesicles, called exosomes, released by mesenchymal stem cells helped to ease vascular remodeling in a rat model of pulmonary hypertension (PH), a study reports.
The study “Mesenchymal stromal cell-derived exosomes improve pulmonary hypertension through inhibition of pulmonary vascular remodeling” was published in the journal Respiratory Research.
Vascular remodeling, a hallmark of PH, is marked by a proliferation of abnormal smooth muscle cells and a loss of endothelial cells (those lining the interior of blood vessels), promoting an imbalance in blood pressure and ultimately PH.
Previous studies suggested that mesenchymal stem cells (MSCs) produce exosomes that help to reduce vascular remodeling. Exosomes are small vesicles released by cells that transport proteins and nucleic acids, like RNA and DNA, to other cells. When receiving cells interact with exosomes, they react to their cargo and can change their behavior.
The molecular mechanisms underlying the benefits of MSCs-exosomes in PH, however, remain unknown.
A team led by researchers at The Second Hospital of Shandong University, in China, investigated how exosomes derived from MSCs lessened vascular remodeling in a rat model of PH, the monocrotaline-induced PH rat model.
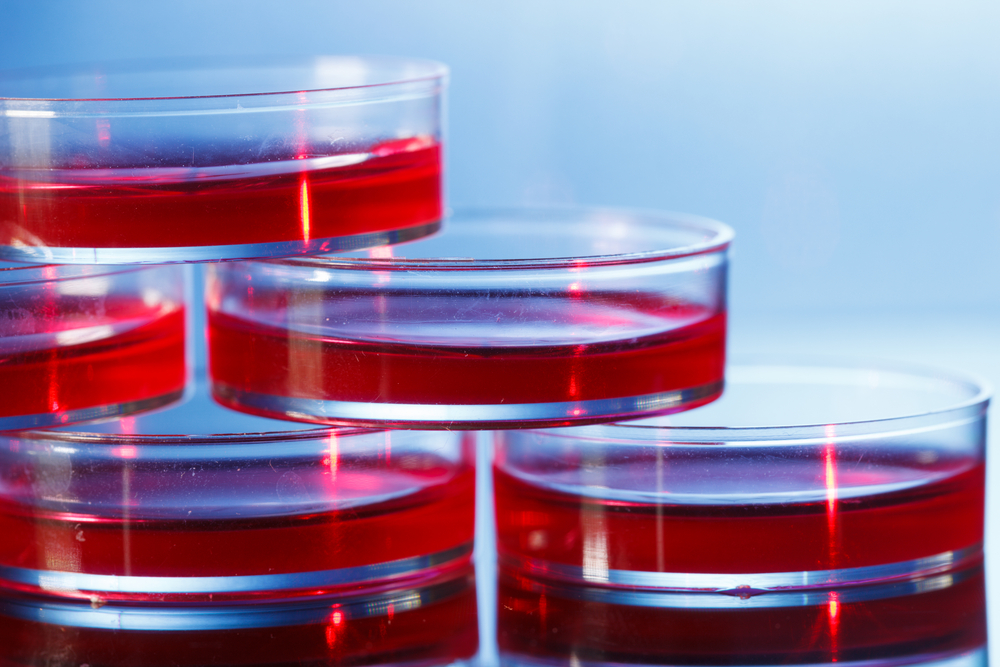
The group cultured MSCs derived from human umbilical cords to obtain exosomes.
Researchers began by testing whether MSC exosomes interacted with endothelial cells. They confirmed that MSC-exosomes were indeed taken up by pulmonary arterial endothelial cells (PAEC).
They then injected MSC exosomes into rats in the PH model.
The animals showed a significant reduction in pulmonary vascular remodeling, and in right ventricle damage to the heart, compared to untreated rats or rats treated with an MSC-culture medium only.
Treatment with MSC exosomes also lessened vessel wall thickness and right ventricle enlargement, and the degree of scarring (fibrosis).
At the cellular level, exosomes reduced the levels of a gene whose protein, α-smooth muscle actin (α-SMA), promotes fibrosis, while increasing levels of CD31, a surface protein used to identify endothelial cells.
Further molecular analysis revealed that MSC exosomes enhanced the levels of Wnt5a, and decreased those of beta-catenin and its target cyclin D. Wnt5a, a protein part of the Wnt signaling pathway, is known to reduce the proliferation of smooth muscle cells and to increase the proliferation of endothelial cells. (The Wnt pathway regulates beta-catenin, a protein that drives cell proliferation and cell migration.)
To better understand how Wnt5a was acting on pulmonary arterial muscle cells (PAMSC) and PAEC ( pulmonary arterial endothelial cells), researchers tested how this protein changed with hypoxia (low oxygen levels when blood supply is impaired).
Hypoxia was seen to decrease Wnt5a expression, and MSC exosomes treatment was able to restore its levels.
Researchers also noticed that Wnt5a had an anti-apoptotic effect when cells were grown under hypoxic conditions. Apoptosis is the term used to describe programmed cell death. So the findings indicate that Wnt5a protected PAEC cells from dying.
Next, the team investigated the effects of exosomes in migration and tube formation ability of PAECs. They observed that treating cells with exosomes enhanced their tube and capillary network formation; their ability to migrate was also boosted by exosomes.
Better cell adhesion and contraction abilities were also evident in PAECs treated with exosomes.
In turn, MSC exosomes prevent PAMSC proliferation under hypoxic conditions.
These findings indicate that MSC exosomes modulate endothelial and muscle cells behavior via Wnt5a, and suggest that this mechanism may offer a new way of treating PH.
“The present study suggest that MSC-exo [exosomes] can significantly upregulate the expression of Wnt5a in MCT-PH rats and hypoxic pulmonary vascular cells,” to “attenuate PH pulmonary vascular remodeling,” the researchers wrote.
However, the molecular mechanisms “cannot be clarified in the present study and would need further investigations,” they added.