Chloride Channel TMEM16A May Be Therapeutic Target for IPAH, Study Suggests
Patients with idiopathic pulmonary arterial hypertension (IPAH) have greater levels and activity of a chloride channel known as TMEM16A, which contributes to disease-related changes in pulmonary cells, according to a new study.
The findings also revealed that long-term treatment with benzbromarone, a TMEM16A blocker, induces relaxation of blood vessels and lessens vascular remodeling in animal models of pulmonary hypertension.
The research was published in a study, “Targeting TMEM16A to reverse vasoconstriction and remodelling in idiopathic PAH,” in the European Respiratory Journal.
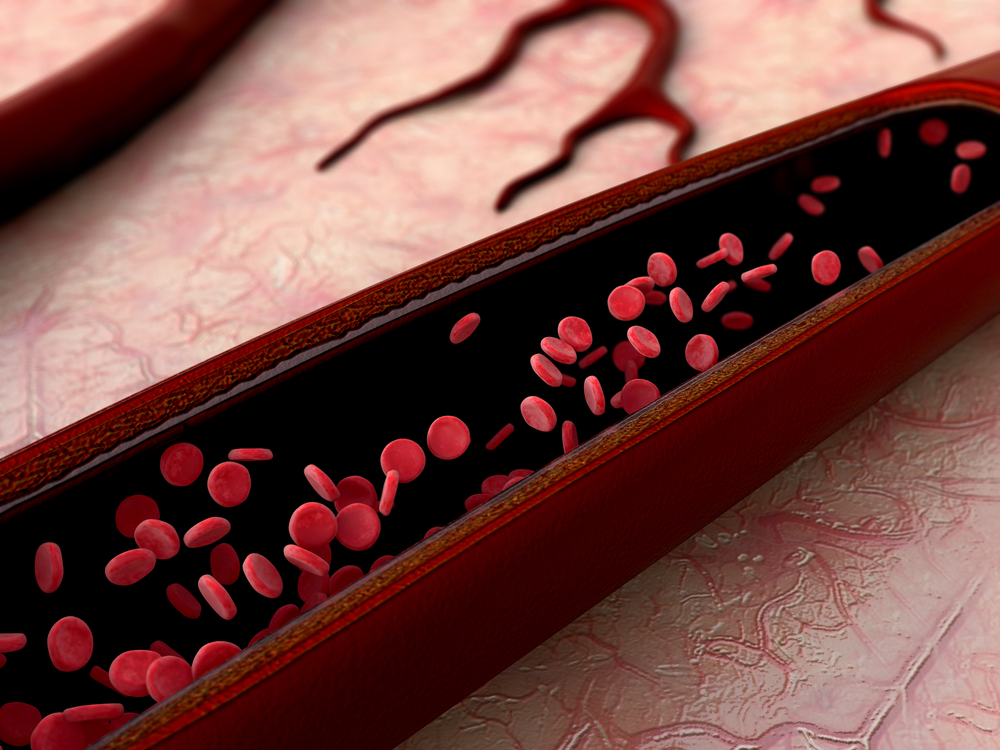
IPAH is characterized by vasoconstriction, or blood-vessel tightening, and associated remodeling. At the molecular level, different ion channels and transporters, as well as calcium-handling proteins, show altered production and function.
The calcium-activated channel TMEM16A is active at the resting cell membrane in pulmonary arterial smooth muscle cells (PASMCs). When these channels open, chloride exits the cells, the membrane’s potential changes (a process called depolarization), and calcium enters. However, the function of TMEM16A in human PASMCs and its involvement in pulmonary disease are not well understood.
Now, an international team from Austria, Hungary, and Germany has shown that both the levels of messenger RNA (mRNA) — molecules produced from DNA — and protein function of TMEM16A were significantly increased in IPAH patients. This was tested in lung samples obtained from IPAH patients and controls in a Phase 2 trial (NCT02790450) testing benzbromarone. In contrast, the levels of the chloride channel CFTR were lower in IPAH patients.
Join the PH forums: an online community especially for patients with pulmonary hypertension.
The TMEM16A upregulation was associated with an increased chloride current, or flow, in cells from IPAH patients. Exposing healthy cells to hypoxia — low oxygen amounts — induced these IPAH features, including both the increased amount of TMEM16A and the greater chloride current.
The researchers then found that suppressing the ANO1 gene, which contains instructions to make TMEM16A protein, lowered the channel’s mRNA and protein levels, and also decreased the chloride current in PASMCs.
Treatment with benzbromarone (a TMEM16A inhibitor) also reduced this chloride current, while normalizing the resting membrane potential of cells derived from IPAH patients.
In addition, overexpressing TMEM16A depolarized human PASMCs, an effect reversed by benzbromarone.
Subsequent experiments revealed that benzbromarone caused a dose-dependent vasorelaxation in mouse and rat pulmonary arteries. In vivo, benzbromarone led to a significant decrease in right ventricular systolic pressure (RVSP) in mouse and rat models of pulmonary hypertension (PH).
“Chronic application of benzbromarone in two independent animal models significantly decreased right ventricular pressure and reversed remodelling of established PH,” the researchers wrote.
In addition, experiments in eight patients with severe IPAH showed that oral treatment with 200 mg of benzbromarone — the maximum approved single oral dose for the prevention of gout with this therapy — did not have acute vasodilatory effects, “probably due to low benzbromarone plasma concentrations and a very short exposure time,” the team wrote.
To further assess the efficacy of benzbromarone to reverse vascular remodeling, the scientists administered the treatment via under-the-skin slow-release pellets to mice and rats with PH. Benzbromarone significantly decreased RVSP, pulmonary artery remodeling, and right ventricular hypertrophy or enlargement.
Assessments in mouse and rat lung sections revealed that treatment with benzbromarone reduced the proliferation of PASMCs. Conversely, overexpression of TMEM16A increased PASMC proliferation.
“Our findings suggest that increased TMEM16A expression and activity comprise an important pathologic mechanism underlying vasoconstriction and remodeling of pulmonary arteries in PAH,” the researchers wrote.
The team suggested that blocking TMEM16A “represents a novel therapeutic approach to achieve reverse remodeling in PAH.”