CMR Fluoroscopy Right Heart Catheterization Superior to More Common Techniques for Hemodynamic Testing
A new study shows that CMR (cardiovascular magnetic resonance) fluoroscopy-guided heart catheterization is a safe method with an appropriate procedure time, high rate of success, and better accuracy than the more commonly used techniques to determine hemodynamic parameters.
The study, titled, “CMR fluoroscopy right heart catheterization for cardiac output and pulmonary vascular resistance: results in 102 patients,” was published in the Journal of Cardiovascular Magnetic Resonance.
Hemodynamic measures are crucial in determining whether a heart is correctly functioning in cardiopulmonary patients. To conduct a hemodynamic assessment, it is important to quantify cardiac output and pulmonary vascular resistance (PVR).
The most common methods for measuring these parameters are known as thermodilution and the Fick principle, both of which have substantial internal errors and have been shown to be inaccurate more than 25 percent of the time. Fick’s principle uses a complex formula, based on the rate of oxygen consumption per minute and the oxygen concentration in both arteries and veins.
CMR is a validated technique for determining hemodynamic parameters such as cardiac output. In fact, CMR flow measurements of cardiac output and PVR have been shown to be superior to those conducted by Fick’s calculation.
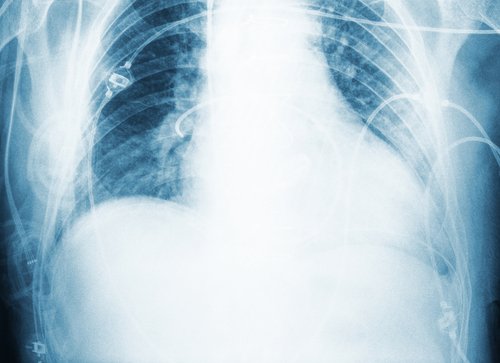
To conduct both PVR and cardiac output measurements at the same time, right heart catheterization (RHC) can be performed using CMR fluoroscopy, which helps guide the catheter to the heart where the physician will be able to conduct a full anatomic assessment as well as determine the hemodynamic parameters.
Researchers at the National Institute of Health conducted CMR fluoroscopy-guided RHC in patients and compared the hemodynamic assessments to those done by the Fick principle under resting conditions and altered circumstances, such as 100 percent inhaled oxygen and nitric oxide.
Researchers report that RHC was successfully performed without complications in 95 percent of patients. The time to conduct this assessment was 20 minutes, plus or minus 11 minutes, which was an acceptable procedure time.
Results showed that the CMR fluoroscopy-guided RHC had a high success rate and demonstrated excellent correlation of hemodynamic parameters with those determined by Fick’s calculations at baseline measurement.
However, the agreement between CMR fluoroscopy-guided RHC and Fick’s principle of the hemodynamic parameters after physiological alterations of 100 percent inhaled oxygen and nitric oxide was less than at baseline. This was due to the inaccuracy of Fick’s principle when there is a lower oxygen difference between the arteries and the veins.
Arteries and veins have different oxygen levels at rest. But if patients inhale 100 percent oxygen, which sometimes happens during tests, the difference is reduced. The findings from this study suggest Fink’s principle cannot obtain reproducible measurements when that is the case.
Study results indicate that CMR catheterization is a promising tool for hemodynamic assessment as it can also be coupled with anatomic assessment. It is particularly a better tool for determining these parameters when patients have been exposed to physiological alterations such as 100 percent inhaled oxygen.







