Imbalance in Gut Bacteria Composition May Play Key Role in PAH
Written by |
An imbalance in the composition of bacteria living in the gut, a phenomenon known as dysbiosis, may play a key role in the onset and progression of pulmonary arterial hypertension (PAH), a study in animals suggests.
The study, “Gut microbiota modification suppresses the development of pulmonary arterial hypertension in an SU5416/hypoxia rat model,” was published in the journal Pulmonary Circulation.
PAH is a progressive disorder caused by the narrowing of the arteries connecting the lungs to the heart, leading to high blood pressure and heart strain. Even though inflammation has been linked to the development of PAH, the exact mechanisms at work during onset and over the course of the disease are still not fully understood.
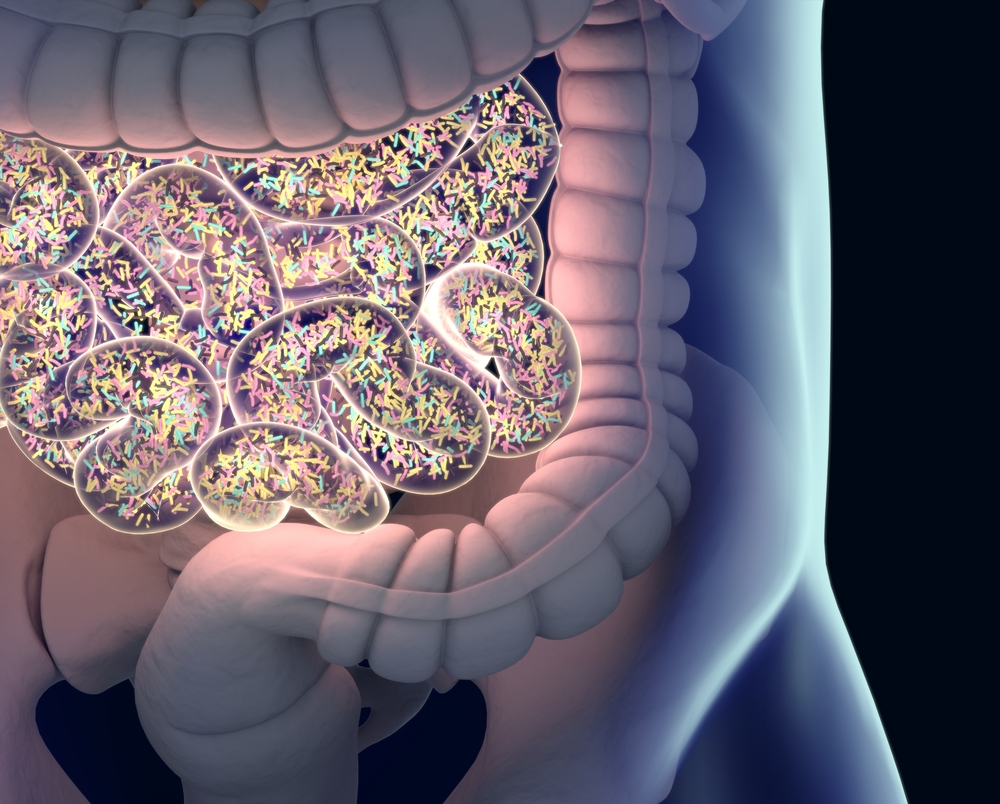
Alterations in the gut microbiome — the group of microbes living in the gastrointestinal tract — of a rat model of induced PAH were reported in a study published in 2018. However, it is still unclear at this point if these changes in gut microbiome composition may be a cause or a consequence of the disease.
To try to answer this question, investigators in Japan used a combination of antibiotics to change gut bacteria composition in the same rat model of induced PAH. After doing so, they examined if and how these alterations affected several disease parameters in the animals, including blood pressure, and heart and blood vessel structure.
First, the team triggered the onset of PAH in the animals by injecting them with SU5416, a pharmacological inhibitor of a protein receptor that is needed for the normal development of cells lining the inside of lung blood vessels. They then kept the rats in special chambers containing low concentrations of oxygen (about 10%) for three weeks.
Over this period of time, some rats also were treated with a combination of four different antibiotics — ampicillin, vancomycin, neomycin, and metronidazole — to alter their microbiome composition, while others received no treatment.
The investigators also included two other groups of animals: some that were never injected with SU5416 but were kept in low-oxygen chambers for three weeks; and healthy untreated rats that were used as controls.
Bacterial DNA from stool samples taken from the four groups of rats was then isolated and a series of molecular and gene sequencing analyses were used to identify the species of bacteria living in the animals’ GI tracts.
Compared with the healthy rats, those with induced PAH that were not treated with antibiotics had a significantly higher Firmicutes-to-Bacteroidetes (F/B) ratio, which is commonly used as a marker of dysbiosis. A higher F/B ratio indicates that animals had more bacteria belonging to the Firmicutes phylum than Bacteroidetes in their GI tract.
In addition, 14 genera of bacteria, including Rothia and Prevotellaceae, were found to be more abundant in rats with induced PAH than in the healthy animals, while six, including Bacteroides and Akkermansia, were found in lower amounts in the PAH-induced rats than in the controls. According to the researchers, these imbalances may play a role in either the induction or suppression of inflammation, which could be linked to PAH development.
As expected, rats with induced PAH that had been treated with antibiotics for a month had a much lower number of bacteria living in their GI tract than those of the other three groups.
The investigators also discovered that, compared with rats with PAH that received no antibiotic treatment, those that had been treated with antibiotics had lower blood pressure in the right ventricle, which is the right lower side of the heart that normally pumps blood to the lungs.
Moreover, the findings showed that antibiotic treatment seemed to prevent the enlargement of the heart’s right ventricle, which tends to happen over time as PAH progresses. Antibiotic treatment also lessened blood vessel narrowing and obstruction in the animals’ lungs, another key hallmark of PAH.
According to the researchers, these findings suggest that alterations in the composition of gut bacteria caused by antibiotic treatment prevent, at least to a degree, the development of PAH.
“Dysbiosis may play a causal role in the development and progression of PAH, and modification of gut microbiota might be a new option for the prevention of PAH,” they concluded.