$2.67M grant to explore why HIV increases risk of PH
4-year grant was given to Sharilyn Almodóvar at TTUHSC School of Medicine
Written by |

A research project to help shed light about why people with the human immunodeficiency virus (HIV) are at higher risk for developing pulmonary hypertension (PH) was awarded a $2.67 million grant.
The four-year grant from the National Heart, Lung and Blood Institute, part of the National Institutes of Health, was given to Sharilyn Almodóvar, PhD, at the Texas Tech University Health Sciences Center (TTUHSC) School of Medicine.
Titled “Role of HIV gp120 and Nef in Transcriptome Dysregulation and Pulmonary Vascular Remodeling,” the project will investigate how HIV perturbs the complex interactions between the different cells of the lung arteries. HIV is the virus that causes AIDS.
A feature of PH is high blood pressure in blood vessels that supply the lungs, known as the pulmonary arteries. As a result, the heart’s right ventricle must work harder to pump blood. A PH diagnosis may take several tests, including a right heart catheterization, an invasive procedure that measures pulmonary artery pressure via a catheter inserted in a vein of the neck, arm, or groin.
PH is more common among people with HIV, the evidence suggests. While “treated patients do not die of AIDS” and “HIV is being treated as a chronic disease, we still do not have a cure, and the longer people live with HIV, the more susceptible they become to comorbidities [coexistent disorders] that affect their quality of life and may even cause premature death,” Almodóvar said in a university news release.
What will the study explore about PH in HIV?
The project will tackle the reasons that underlie the frequency of PH among people with HIV, particularly whether certain mutations in HIV may play a role.
“We do not know how HIV causes or contributes to these severe pulmonary vascular diseases,” Almodóvar said. “With these funded studies, we will increase the understanding of how HIV changes the way that the cells in the lung interact with this virus so that we can propose novel therapies to prevent lung diseases in people with HIV.”
“Years ago, we had the opportunity to study the virus in nonhuman primates and in patients diagnosed with pulmonary hypertension associated with HIV, and we discovered specific mutations in the virus,” Almodóvar said. “With this new study, we will examine how these mutations in the virus damage the normal interactions between different cell types in the lung arteries.”
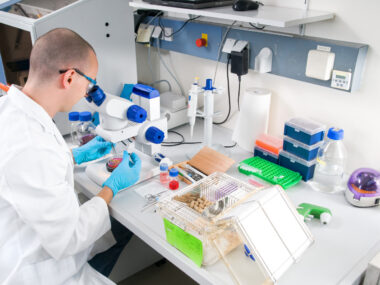
The researchers plan to use a mouse model that carries a humanized immune system, meaning mice engrafted with human cells and tissues. This model enables exploring the interactions between HIV and human immune cells and how this affects pulmonary blood vessels.
After infecting the mice with HIV, the researchers will monitor its progression to assess the number of viruses in the blood — or viral load — along with the number of CD4-positive T-cells, key immune cells targeted by HIV and depleted in AIDS. Markers of inflammation in circulation will also be measured.
“At the end of each experiment, which takes months to complete, we perform right heart catheterizations on these mice to measure their pulmonary arterial pressures and examine their hearts for evidence of heart disease,” said Almodóvar, who will work with a multidisciplinary team that will include scientists at TTUHSC and a collaborator at Vanderbilt University.