New Case-Study Highlights PAH-associated with Systemic Lupus Erythematosus
In a recent study entitled “Lupus-Associated Pulmonary Arterial Hypertension: Variable Course and Importance of Prompt Recognition”, researchers present a case study of a young woman with systemic lupus erythematosus (SLE) exhibiting pulmonary arterial hypertension, a potentially lethal SLE-manifestation. They highlight the need for a prompt recognition of PAH in SLE patients so that effective treatment can be introduce promptly and prevent SLE patients’ deaths. The study was published in the journal Case Reports in Medicine.
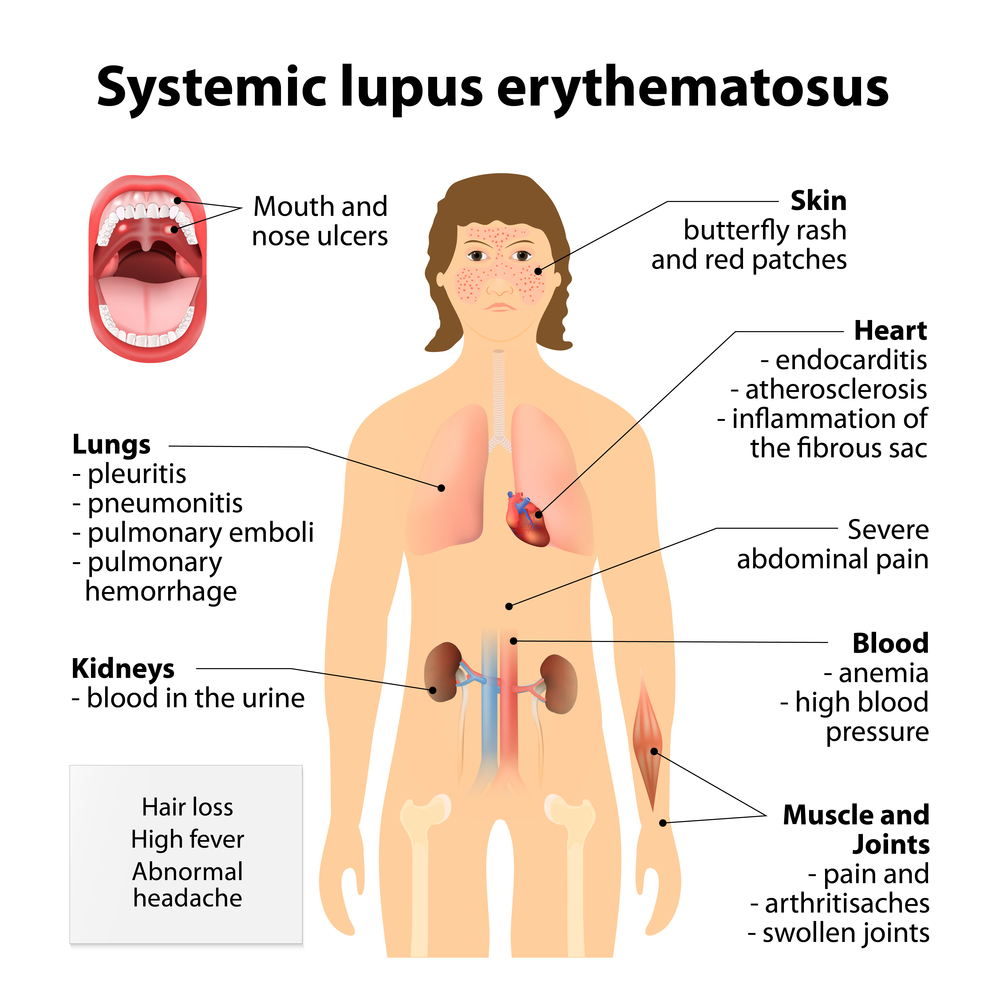
Systemic lupus erythematosus (SLE) is an autoimmune disease, a disease characterized by the immune system attacking the body’s own tissues, which can affect several organs, including skin, joints, kidneys, lung, and the nervous system. Women have a higher risk for developing SLE compared to men, with African Americans and Asians being particularly susceptible. Its symptoms, although varying from person to person, usually include joint pain and swelling; some develop arthritis; other symptoms include skin rash (actually, a “butterfly” rash is common in SLE patients, approximately 50%, and is often occurring in the over the cheeks and over the nose, but can occur widespread over the body).
A lethal manifestation of SLE can be pulmonary arterial hypertension (PAH), often leading to SLE patients’ death. The prevalence, however, of SLE patients affected with PAH is currently unclear, with previous studies pointing a range between 0.5 to 43%; more recent studies have narrowed it down to 0.5 to 17.5%.
In this new study, authors describe a case report of a 25-year-old woman with SLE and presenting with circulatory shock, multi organ dysfunction, and elevated right-sided heart pressures. She was later diagnosed with acute severe pulmonary arterial hypertension (PAH) whenever she experienced SLE flares.
The authors presented this case to reflect and highlight the necessity for a prompt recognition of severe PAH in SLE patients. Additionally, they point to the variable course SLE-associated PAH may exhibit in the same patient, and so there is the need to address each episode with the most effective treatment. As a result, they conclude that a multidisciplinary team composed of specialists in pulmonary hypertension (pulmonologists and/or cardiologists) and rheumatologists with a vast understanding of SLE is essential for an effective therapeutics. The early recognition of symptoms of PAH in SLE patients is crucial for therapeutics success.







