New Tool Assesses Right Ventricular Dysfunction in PH, Congenital Heart Disease and Cardiomyopathy
Written by |
Right ventricular (RV) dysfunction is a characteristic of several disorders such as pulmonary hypertension, congenital heart disease and cardiomyopathy, making RV function evaluation key to effective prognosis and diagnostic value in such disorders. However, diagnosis through RV function is challenging due to anatomical configuration of the RV. Right ventricular outflow tract (RVOT) is an important measurement of overall RV function. In a new study, researchers in the Department of Pediatrics at Tokushima University evaluated if measurement of pulmonary annular motion velocity could be a reliable and useful tool to determine right ventricular outflow tract (RVOT) performance in pediatric patients with RV dysfunction. The research paper, entitled “Pulmonary Annular Motion Velocity Assessed Using Doppler Tissue Imaging – Novel Echocardiographic Evaluation of Right Ventricular Outflow Tract Function” was published in Circulation Journal.
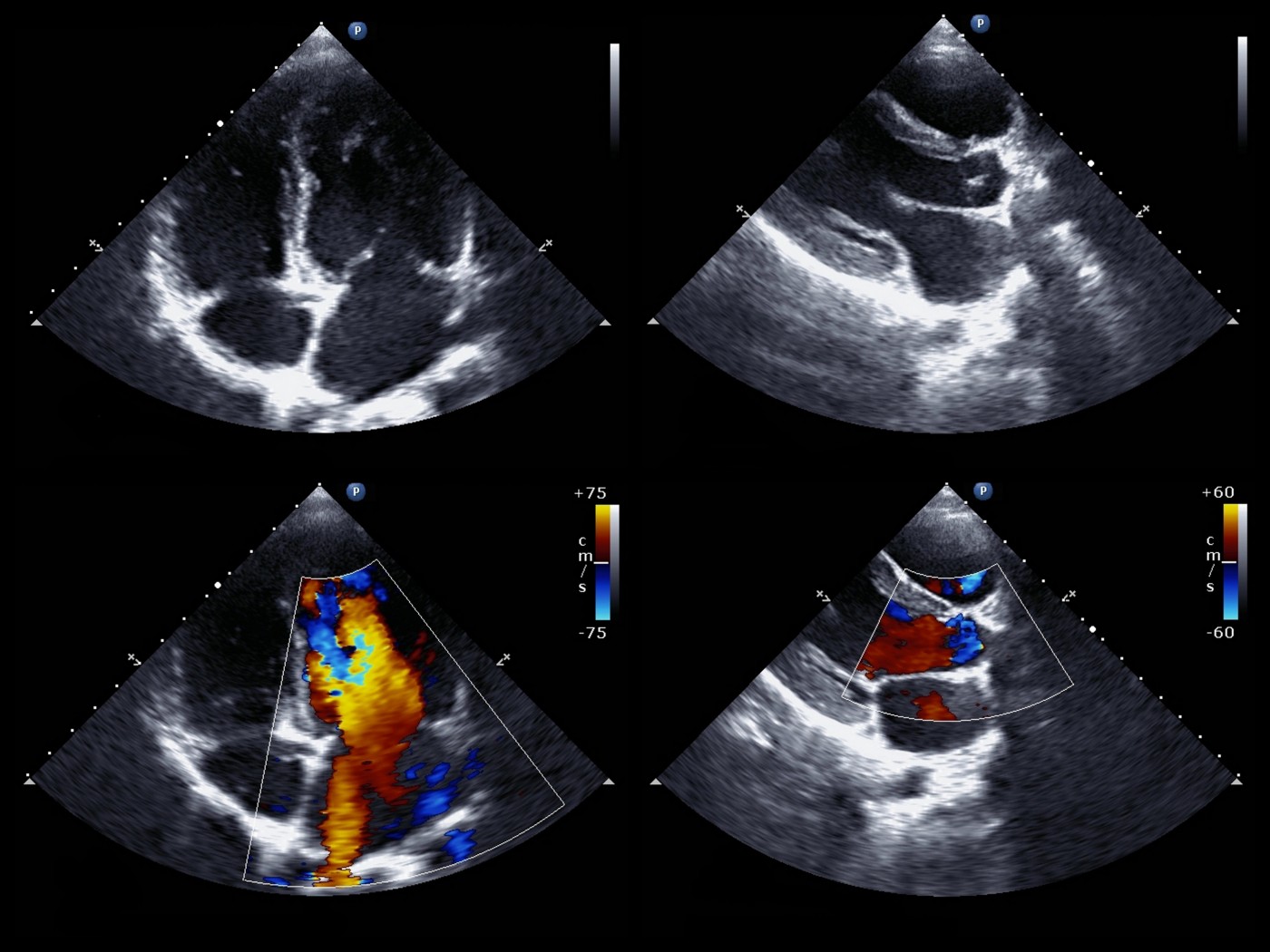
Researchers evaluated RVOT through Tissue Doppler Imaging (TDI) a method to measure tissue velocity in children aged 5 to 10 years who were diagnosed with several heart defects: 16 patients with preoperative atrial septal defect (ASD), 6 patients with pulmonary arterial hypertension (PAH) and 32 children with surgically repaired tetralogy of Fallot (TOF). A control group of 40 healthy children was used for comparison. The Doppler data was obtained through standard and pulsed Doppler tissue echocardiography, where pulmonary annular motion velocity and tricuspid (heart valve) motion velocity parameters were measured during three heart cycles.
The evaluation results revealed that pulmonary annular motion velocity obtained through TDI is a valuable tool for assessment of RVOT function. The evaluated waveforms included systolic bimodal (s1’ and s2’) and diastolic e’ and a,’ all with distinct profiles according to disease type and between disease and control groups. The peak velocity of s1’ and s2’ was significantly higher in the ASD patients, who generally preserve RV function, than in the controls, a result compatible with previous studies.
RELATED: Highlights on New Theory for Pulmonary Arterial Hypertension: The Metabolic Theory
In the PAH group, the peak velocity of the s1,’ s2,’ e,’ and a’ waves was significantly lower than in the control group. Because tricuspid velocity presented no significant decrease, researchers theorize the pulmonary annular motion velocity might identify patients with reduced RV systolic function more accurately than the tricuspid annular measurement, a parameter that has been associated with overall motion of the heart and not specifically RV contraction. TOF patients presented similar decreased velocity values in s1,’ s2,’ e,’ and a’ waves when compared to control group.
Overall, the research study suggests that pulmonary annular velocity reflects and is a promising diagnostic tool for RVOT performance in various cardiac diseases and provides detailed insight into right ventricular dysfunction. The tool could be used in the future to further improve diagnosis of PH, which can be elusive. The earlier that pulmonary hypertension is diagnosed in patients improves overall patients outcomes in terms of quality of life and lifespan, making improved diagnostic approaches a much-needed advancement in the field.



