PADN effective for PH, meta-analysis of studies shows
Procedure lowers blood pressure in lungs, improves heart function
Written by |
Pulmonary artery denervation (PADN), a procedure that targets overactive nerves involved in blood vessel constriction, significantly lessens high blood pressure in the lungs of people with pulmonary hypertension (PH), according to a meta-analysis of more than a dozen studies.
Pooled data also showed that the approach was associated with significant improvements in heart function and exercise capacity, further supporting its “promise as a therapeutic intervention for PH,” the researchers wrote.
“Pulmonary artery denervation has become a promising therapeutic intervention in the management of pulmonary hypertension,” James Jenkins, MD, study co-author and a cardiologist at Ochsner Health System, said in a Ochsner Health press release. “While our findings suggest a substantial role for PADN in treatment protocols, continuous research is crucial to fully understand its broader implications and long-term benefits.”
The study, “Pulmonary artery denervation in pulmonary hypertension: A comprehensive meta-analysis,” was published in the International Journal of Cardiology.
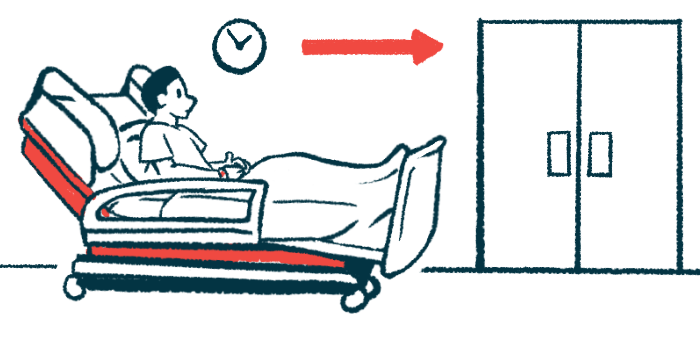
In PH, high blood pressure in the pulmonary arteries, the blood vessels that supply the lungs, makes it more difficult for the right side of the heart to pump blood to the lungs. This can lead to PH symptoms including shortness of breath during routine activities.
‘Potential game-changer’
“Conventional treatments primarily include vasodilators [blood vessel-widening medications], which provide symptomatic relief but do not effectively reverse the underlying [blood vessel abnormalities],” the researchers wrote.
PADN has in recent years “emerged as a potential game-changer in the treatment landscape of PH,” they wrote.
The procedure uses heat or radio waves to disable overactive nerves around the pulmonary arteries. This should help relax these blood vessels, lowering blood pressure and making it easier for the heart to pump blood to the lungs.
To better understand the benefits of PADN in PH patients, the researchers used a method called meta-analysis to combine data from studies published up to September 2023 and reporting on outcomes of PH patients treated with the procedure.
A total of 14 studies, covering 372 patients, were included in the final meta-analysis. The methods used, follow-up times, and outcomes evaluated differed from study to study.
The meta-analysis’ main goal was to watch for changes in a range of blood-related measures, including mean pulmonary artery pressure (mPAP); pulmonary vascular resistance (PVR), the resistance that must be overcome for blood to flow to the lungs; and mean right atrial pressure (mRAP), the pressure in the right upper chamber of the heart.
All 14 studies reported data on mPAP and PVR, and pooled data showed a significant decrease in both parameters after PADN. However, there was high variability across studies.
Eight studies, with a total of 276 patients, reported consistent results about mRAP, which also decreased significantly after PADN.
Data from 13 studies (360 patients) showed that PADN helped the heart pump significantly more blood. In nine studies (226 patients), the approach was also reported to significantly increase the distance patients could walk in six minutes, a common test for exercise capacity. The studies for each outcome showed some degree of variability among them.
“Our meta-analysis provides insight into the changing field of PADN as an upcoming treatment option for PH,” the researchers wrote. “However, the ongoing differences in patient responses and procedure modifications highlight the complex and subtle character of the results.”
That points to the need for clear guidelines on standard PADN procedures and larger, long-term, appropriately controlled clinical trials to confirm the results and identify patients who would benefit most from the procedure, the team said.


