PAH Patients Exhibit Skeletal Muscle Abnormalities; Underlying Mechanisms Remain Unknown
In a new study entitled “Signaling pathways underlying skeletal muscle wasting in experimental pulmonary arterial hypertension,” researchers investigated the potential mechanisms underlying patients with pulmonary arterial hypertension characteristic skeletal muscle abnormalities. The researchers identified that muscle loss is prompted by accumulation of dysfunctional mitochondrias and ineffective removal of damaged proteins, leading to muscle cell loss and enhancing muscle atrophy. The study was published in the journal Biochimica et Biophysica Acta (BBA) – Molecular Basis of Disease.
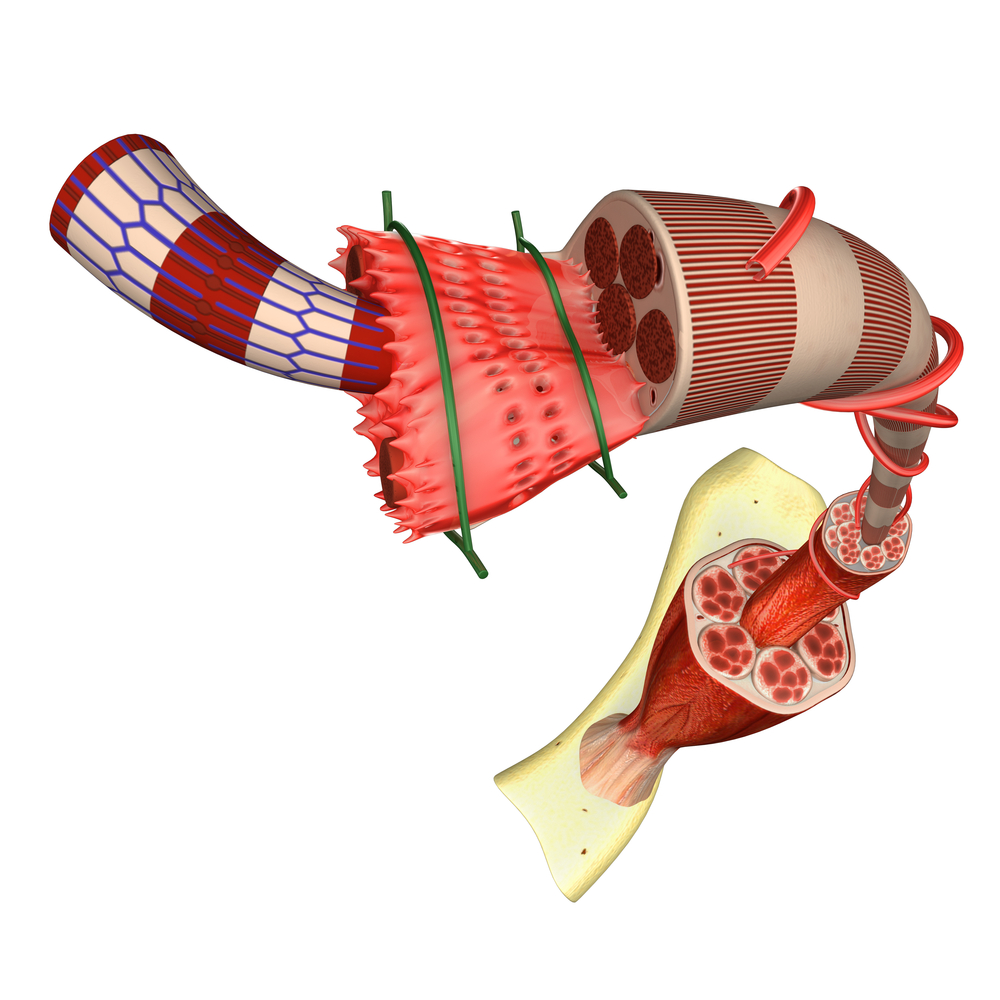
Pulmonary Arterial Hypertension (PAH) is characterized by increased blood pressure in lung arteries due to their abnormal constriction, and includes shortness of breath, dizziness, fainting, and leg swelling as main symptoms. Due to inefficient cardiac and respiratory systems, PAH patients’ exercise capacity is severely impaired, determined by abnormally low oxygen levels in the blood, right ventricular hypertrophy, and skeletal and respiratory muscle weakness.
Recent studies have suggested that PAH patients harbor intrinsic skeletal muscle abnormalities, but the mechanisms underlying PAH-related muscle weakness and waste are still far from clear. In this new study, authors investigated these mechanisms further using an animal model of PAH induced by monocrotaline (MCT, induces endothelial injury leading to vascular remodeling and pulmonary hypertension and mimics most of PAH pulmonary and cardiac features).
The authors randomly assigned rats to receive either saline or MCT injections (60mg/Kg), and within four weeks of injection the rats were anesthetized and submitted to right ventricular (RV) hemodynamic tests. They observed that MCT-induced PAH animals develop significant skeletal muscle loss, which was associated with an increase in several catabolic markers (both local and systemic). The team also discovered that muscle wasting was associated with a significant loss of mitochondria activity. Specifically, they found decreased mitochondrial ATP synthase expression and activity as well as reduced Tfam and paraplegin expression, suggesting an accumulation of dysfunctional mitochondria in skeletal muscle.
RELATED: Targeted Therapeutics Under Investigation For PAH Treatment
The team identified evidence of anabolism/catabolism imbalance associated with MCT-induced muscle loss, which they suggest may be attributed to the increase of pro-inflammaroty cytokines that characterize PAH patients. Additionally, the accumulation of damaged mitochondria and an inefficient mitochondria protein quality control system that is incapable of removing damaged proteins contributes to muscle loss — potentially by impacting the health of muscle cells and triggering the release of pro-apoptotic factors and reactive oxygen species, damaging the muscle even further.







