Bariatric Surgery Improves PAH in Patients with Obesity
Written by |
Obesity is a prevalent comorbidity of pulmonary arterial hypertension (PAH), according to a recent study that examined the presence of metabolic syndrome in patients with PAH. In fact, a large body of research has examined obesity-related PAH. However, patients with both of these conditions have hope to improve symptoms of both through bariatric surgery — either gastric bypass or sleeve gastrectomy. As reported by “Improvement in Severe Pulmonary Hypertension in Obese Patients after Laparoscopic Gastric Bypass or Sleeve Gastrectomy,” which was published in Surgical Endoscopy, surgery can improve signs and symptoms of PAH and reduce body mass index (BMI) in the short-term.
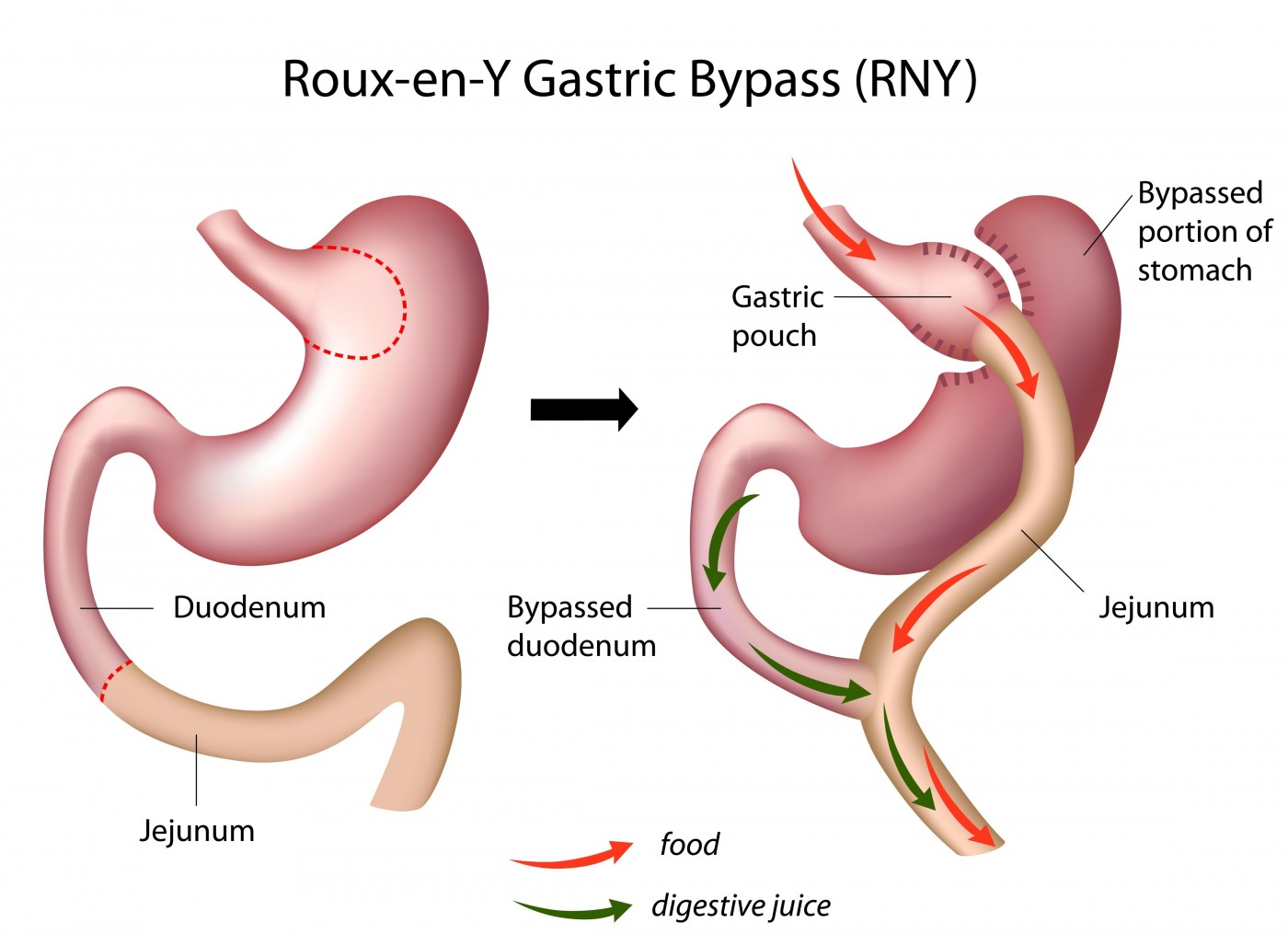
Motivation for the current retrospective analysis came from two case reports of obese PAH patients who underwent laparoscopic gastric bypass surgery and saw dramatic improvements in their pulmonary artery pressures and abilities to exercise. One of the patients had type 1 PAH, and the other had idiopathic PAH. Since the surgery may have contributed to — or been responsible for –their improvements, the authors of the present study examined two cohorts of obese PAH patients at Massachusetts General Hospital. One group received bariatric surgery (either laparoscopic sleeve gastrectomy or laparoscopic Roux-en-Y gastric bypass), and the other received maximal medical therapy. Important to decrease variability and bias in the study, the control and surgery groups were under the care of the same cardiologists/pulmonologists who specialized in PAH, and the surgeries were performed by only six different surgeons.
RELATED: Highlights on New Theory for Pulmonary Arterial Hypertension: The Metabolic Theory
Baseline patient parameters were similar, except that the patients receiving medication without surgery were significantly older by eight years. This control group also tended to need advanced vasodilatory therapy at baseline more than the surgery group. Yet when looking at the two groups of patients at an approximate time of two years following baseline, there was a clear difference.
Breaking patients into three groups based on medication, more patients receiving surgery improved than those in the medication only group. Only one patient who received surgery in the advanced vasodilator therapy group worsened, and this was the only surgery patient reported to have worsened. In the medication only group, 38% of vasodilator therapy patients, 75% of diuretic therapy patients, and 50% of supplemental oxygen patients worsened. This is compared to the 67% of advanced vasodilator therapy patients, 86% of diuretic therapy patients, and 75% of supplemental oxygen patients in the surgery group who improved at the follow-up.
Concerning hematological parameters, surgery seemed to help patients cut their post-mean PAP by nearly half that of the medication-only patients’ PAPs and post-right ventricular systolic pressures (RVSPs). It is unclear whether patients in different classes of PAH benefited more than others due to the small sample size in the study.
Overall, the authors believe there is plenty of evidence to conduct a larger-scale study and analysis to determine how bariatric surgery can be used to manage PAH in obese patients. This would be a valuable study, as the indicated patients are considered high-risk and generally require additional disease management than medication alone.



