Blood Vessel Protein May Predict Lung Hypertension Severity and Response to Therapy
Written by |
Patients with pulmonary hypertension (PH) have much higher levels of the blood vessel factor TSP-1 in their blood, with levels coinciding with the type and severity of the disease.
Since the factor is known to interact with several PH treatment targets, the study, titled “The role of circulating thrombospondin-1 in patients with precapillary pulmonary hypertension“ and published in the journal Respiratory Research, also suggested that more research is needed to evaluate if the protein might, in fact, prevent a therapy from working optimally.
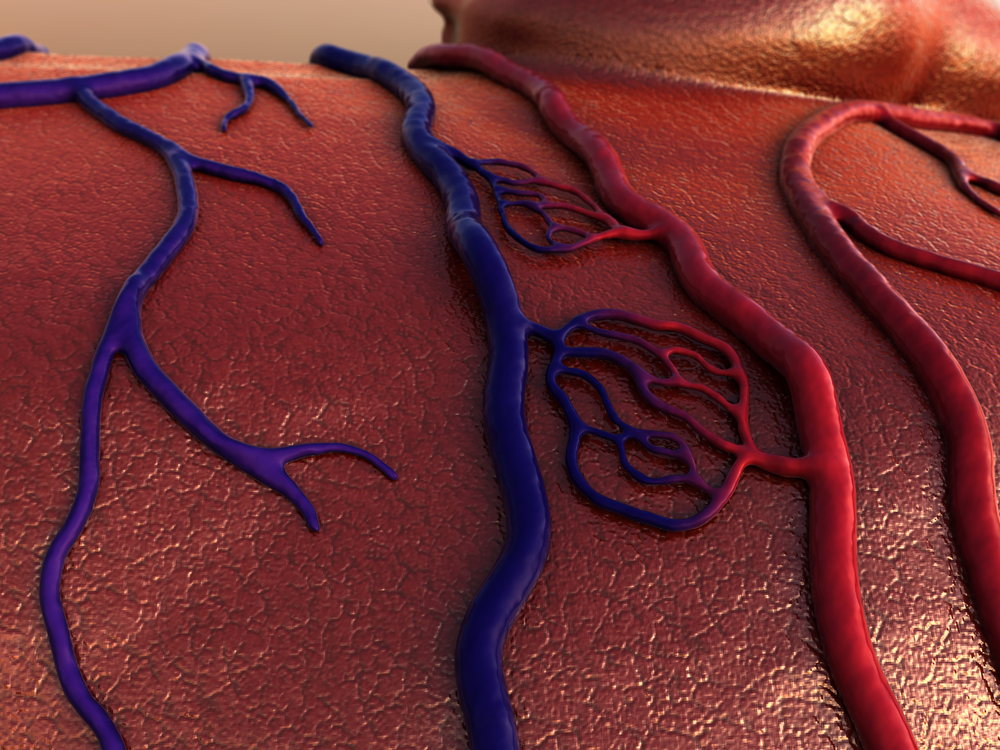
Scientists have been looking at TSP-1’s role in pulmonary hypertension for awhile. In fact, it is well-known that both low oxygen levels and the stress imposed on blood vessels by the pressure of the passing blood trigger this protein’s production, and it can be produced by numerous cell types in blood vessels. The protein’s production is also ramped up if levels of growth factors increase — with all of the above examples of conditions present in lung hypertension.
Increased levels of TSP-1, in turn, also contribute to the hypertensive condition, triggering cell death and disrupting nitric oxide and other growth factors needed for healthy blood vessels. It also triggers tissue fibrosis.
Researchers at Saarland University in Germany wanted to find out if the levels of this protein in the blood could be linked also to disease symptoms and clinical signs. Recruiting 93 patients and 19 controls, they examined levels of TSP-1 and conducted extensive physical and lab examinations.
The patient group consisted of various types of lung hypertension, including pulmonary arterial hypertension (PAH) patients, hypertension linked to chronic lung disease, and lung hypertension caused by chronic blood clots in the lungs, a condition often referred to as CTEPH. Most patients were classified as either WHO functional class II or III.
Levels of TSP-1 were higher among patients than controls, and those with hypertension linked to lung disease had the lowest levels. Levels of the blood vessel factor in the blood rose with increasing functional class.
Patients treated with phosphodiesterase inhibitors — a drug class often used in pulmonary hypertension — had lower levels of the blood vessel factor, while another common drug class, endothelin receptor blockers, had no impact on the levels. Prostacyclins, conversely, were associated with higher TSP-1 levels. The protein also correlated with other factors known to be involved in lung hypertension.
Researchers also explored if protein levels were tied to measurements of blood pressure in the lungs and to heart, and blood flow parameters, and found that its levels were higher in patients with a high blood pressure and resistance in lung blood vessels, and poorer heart function. Those with high TSP-1 levels also had lower chances of survival at five years.
The study suggests that these initial findings point to the need to explore the factor in larger studies, both to confirm its usability as a marker of disease progression and prognosis, but also to evaluate, in detail, its interactions with drugs used to treat lung hypertension.



