5 Things I Wish I Had Known Before My Transplant

Knowing that transplant was my plan when all else failed, I lacked the curiosity to gather information before making a decision. I focused on survival: More information only increased my anxiety.
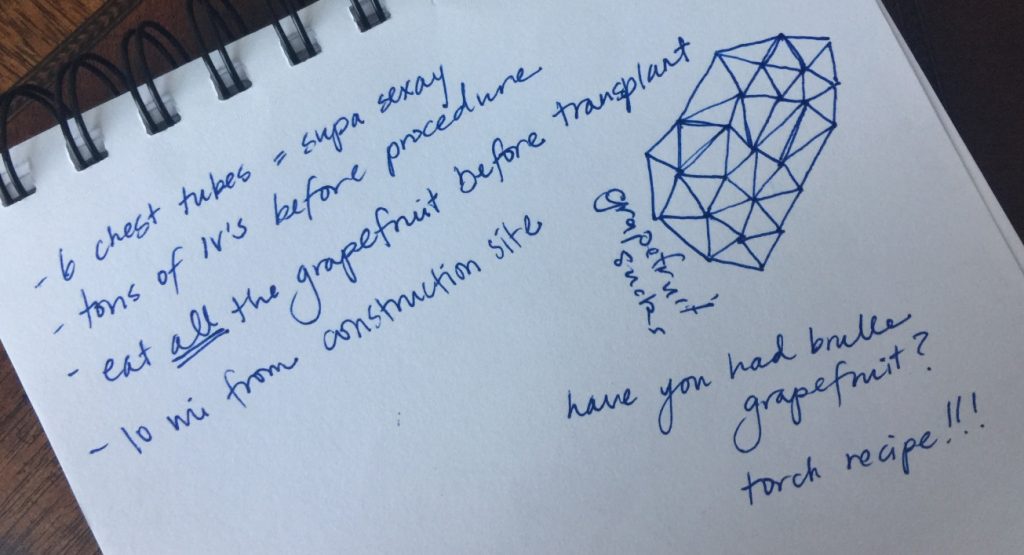
During my training class, I scribbled in a sketchbook and relied on humor to gloss over the enormity of what I was facing. I still don’t wish I had known that my transplant would come with unanticipated and persistent complications, or that it would involve more physical pain than I had experienced before. I could not prepare for those aspects, and knowing they were coming would have only drained my energy to fight them.
If you are willingly reading this column, and transplant may be in your future, I applaud you for being in less denial than I was. Here are a few things I believe I would have benefited from knowing before my transplant:
-
A transplant comes with permanent dietary restrictions.
When I had pulmonary hypertension, I did not appreciate that I could eat anything I wanted (probably because I rarely wanted to eat anything at all). I no longer battle nausea or struggle to maintain a healthy weight, but chronic immunosuppression does come with restrictions.
Grapefruit interferes with immunosuppressants (and many other medications), but that was easy to give up since I don’t regularly encounter grapefruit in restaurants or at friends’ homes. I didn’t learn until after my surgery that all meats must be hot within an hour of consumption. That means no sushi. No cold cuts. Ever again. Had I known this before, I would have found a nice spot to park my oxygen concentrator and started pigging out on spicy tuna rolls and deli sandwiches.
-
Chest tube scars heal.
While listed for transplant, one of my main preoccupations was the impact chest tube scars would have on my body image. I already had a chest tube scar from one open-heart surgery, and I wasn’t fond of it. Chest tubes would be better labeled chest hoses — they’re huge! But my chest tube scars healed, and they look more like an awesome tattoo than six additional blemishes to my already scarred torso. Honestly, I think I should have more impressive scars to show for the battle I fought.
-
It takes a full year to recover. Don’t kid yourself.
Imagining myself younger, stronger, and more determined than most patients, I assumed I would recover quickly and surpass expectations. But it was a year before I tapered down to the lowest dose of prednisone. A year before my doctors felt comfortable spacing appointments months, instead of weeks, apart. A year before my health stopped being my No. 1 focus and I could find other things to talk and dream about. Transplantation is a lot to process, and faster is not always better.
-
Patients are surviving.
Going into transplant, I had a few friends who had received heart-lung and double-lung transplants, but the longest survivor I knew lost her battle after 12 years. I had less of an optimistic outlook on survival rates than I do now that I know more about the statistics and their inaccuracy. Recipients are alive today who had their transplants when centers first started performing heart-lung transplants (more than 30 years ago), so doctors truly cannot determine a limit for how long these transplants can last.
-
Quality of life does improve.
Oxygenation had far-reaching effects that make me able to say with confidence that my quality of life after transplant is immeasurably better than before transplant. Simply by virtue of spending more hours a day awake, I get more done, appreciate life more, and have more experiences with the people I love. The best part? Joining my parents on hikes and sensing their joy as I speed ahead.
***
Note: Pulmonary Hypertension News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Hypertension News or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to pulmonary hypertension.











Michelle
Thank you for sharing! When do you think someone should start pursuing transplant?
Kathleen Sheffer
My PH specialist was very clear about when I should start talking with the transplant team at my center. For me, it was when I had maxed out on all other treatment options and was still experiencing a decline.
Douglas Knuth
I am not to the point of needing a transplant, but thank you for sharing the information. I will savor the foods I can currently eat! Best wishes to you.
Kathleen Sheffer
So glad you are doing well enough to stay off the list! Physicians learn more every day and I am grateful I was able to postpone my transplant with PH treatments. Keep fighting!
Stacie
I also would have like to have known that I take 4 times the amount of medication that I did. I knew, I was trading one disease for another, and would take pills, but I took 22 pills before and take over 40 a day now. It's so worth it, but that was the only thing I was amazed at!
Barbara. Malcom
How long did you have PH before you started having problems and what were your first problems? Do you also suffer from COPD along with PH?
Kathleen Sheffer
I was diagnosed with PH when I was 6, but I complained of shortness of breath as soon as I could talk. I didn't have COPD with PH, but I know many patients who do. I encourage you to connect with other patients through your specialist or Facebook groups who might be dealing with more similar issues.