Study Identifies Gut Bacteria That May Be Linked to PAH
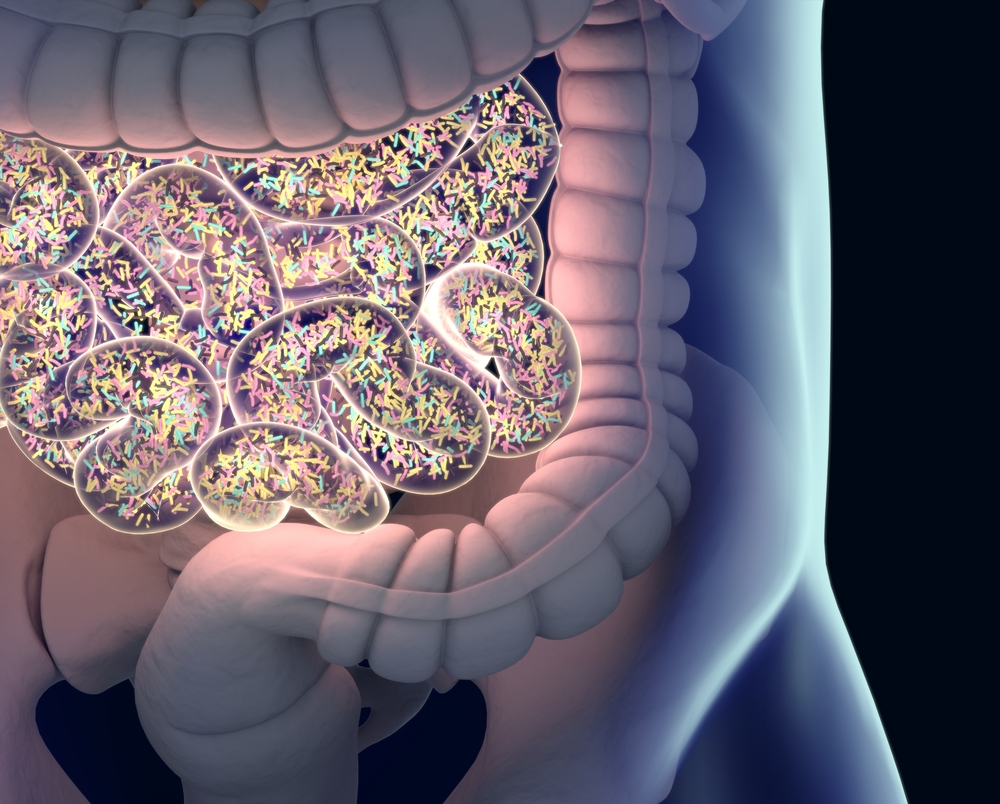
A unique bacterial profile in the guts of patients with pulmonary arterial hypertension (PAH) may contribute to the disease and help predict it, a study found.
The identification of specific microorganisms may lead to earlier, less invasive diagnoses, as well as new avenues for treatment.
The study, “Altered Gut Microbiome Profile in Patients With Pulmonary Arterial Hypertension,” was published in the journal Hypertension.







