Adult PH Patients Share Their Experiences With Transplant Ineligibility
Written by |

When my son Cullen was diagnosed with pulmonary hypertension, people often asked, “Can’t he just get a transplant?” As if he could walk into a hospital, request a heart and a pair of lungs, and be taken right into surgery!
Determining eligibility for transplant is a complicated process of psychological and social evaluations, extensive blood and diagnostic tests, and careful evaluation by a transplant team.
Cullen received a transplant in 2014, but sadly, not everyone is as fortunate. I interviewed three adult PH patients via email, who poignantly explained why they are ineligible for transplant and how they deal with this emotionally.
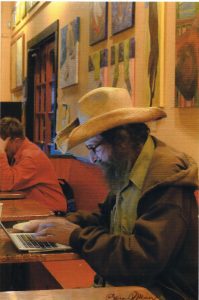
Mendo Buckner, 67, went through the lung transplant eligibility process in 2014 due to chronic obstructive pulmonary disease and emphysema. A right heart catheterization revealed that he also has PH.
He was listed for transplant, but unforeseen circumstances left him without a caregiver capable of meeting the post-transplant requirements. Mendo needed a caregiver who could commit to six months or more of around-the-clock care. He considered hiring someone, but his transplant center does not allow paid nurses as caregivers.
Mendo felt ambivalent about transplant, so when he was removed from the list, he teetered between disappointment and relief.
“The fact that I’ve outlived the average life expectancy of a lung transplant recipient,” Mendo elaborated, “makes me feel even better about it 6 years later.”
Mendo points out that transplant is like trading one disease for another. “For every success story about a 10+ year survivor, there is another who dies within a year or two.”
In addition to potentially serious post-transplant health complications, Mendo also considers the cost. “Medicare doesn’t always cover the post-transplant medications,” he wrote. “Many patients are in a constant struggle with insurance or dependent on Go Fund Me pages or other charities for their survival.”
Jen Cueva, 47, a fellow columnist and forums moderator here at Pulmonary Hypertension News, was diagnosed with PH around the age of 30. Her emotions remain raw since discovering her ineligibility at the end of last year while battling COVID-19.
Her kidneys completely failed, and a transplant was denied because of needing both kidneys and lungs. Jen needed a miracle, or as she put it, “A new body.”
Jen believes that because of the prayers of many, she received her miracle. Her kidneys started functioning enough to help her improve and return home.
She admits feeling anger and frustration about being ineligible for transplant. Acceptance of her body and its limitations continues to wax and wane.
If you are told that you are ineligible for transplant, Jen recommends seeking multiple opinions rather than just one. “Also keep in mind,” Jen said, “that inclusions and exclusions often change.”
But if the answer remains no, Jen stresses the importance of taking the time to process your emotions. “It is not easy, but you can do this!” she wrote.
Tracey Lawrence, 51, was diagnosed with PH in 2019. She is currently ineligible for transplant because of systemic lupus erythematosus, dermatomyositis, and her weight.
Tracey lives in South Africa, where certain cultural beliefs surrounding organ donation make the eligibility criteria for transplant extremely strict.
She wasn’t horribly upset when transplant was declined. “I wasn’t sure I felt prepared to go through such an enormous procedure with all its inherent risks,” Tracey wrote.
She was even uncertain that she could withstand the surgery, considering how ill she was during the evaluation.
“It’s a double-edged sword,” Tracey explained. She is too ill for the surgery to be a success, but the only way for her to get well enough is to have the surgery.
Time has passed, and Tracey has thought about her options. “I believe that I would be prepared to take the risk and I feel that maybe the surgery and recovery wouldn’t be as bad as I think,” she wrote.
But she remains ineligible for transplant. Tracey does her best to be as healthy as possible and values any small improvement. “I have the philosophy of living every day as best I can. I may not be able to do everything I want, but as long as I’ve done my best, I’m happy.”
She advises others to do everything they can to improve their chances of eligibility. “But don’t beat yourself up if there are things that you can’t do or if progress is slow,” she stressed.
Despite eating a healthy diet, Tracey continues to struggle with her weight. But she isn’t giving up and has learned the value of enlisting help from others. A dietitian helps her maintain healthy food habits, and a pulmonary rehab specialist encourages consistent mobility.
Tracey concluded, “Things can get overwhelming, and you may feel isolated, but you need to remember that you are not alone. There are others who understand what you are going through.”
In my next column, I’ll share the perspectives of pediatric patients’ parents.
***
Note: Pulmonary Hypertension News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Hypertension News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to pulmonary hypertension.






Jill Upshaw
Great article Colleen. I have not been approached about a transplant but that day will probably come. I have a connective tissue disorder but it is not Lupas. I had not thought about that being an issue. I am steadily losing weight. I knew that had to be done. I am so glad that Jenn's kidneys kicked in. When you have PH, you become painfully aware of what many take for granted. I feel so blessed when I have a good day and I am so thankful for each day no matter what.
Colleen Steele
Thank you, Jill! If and when the time comes keep in mind what Jen has advised. Seek multiple opinions and be aware that inclusions and exclusions often change. One hospital might not be equipped to handle certain challenging cases when another might be ready and willing. A no at one facility doesn't always mean it's a no at every location. But hopefully you won't need to cross this bridge any time soon. Keep up the effort to stay well and may you enjoy more good days than bad!