Antioxidant enzyme helps protect lung blood vessels in CTEPH: Study
Boosting PRDX2 levels improves heart, lung function in animal model
Written by |

Levels of the enzyme PRDX2 increase as a protective response in chronic thromboembolic pulmonary hypertension (CTEPH) and help reduce damage to blood vessels in the lungs, a new study in laboratory rats has found.
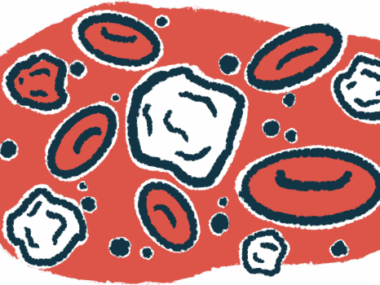
The researchers discovered that the antioxidant enzyme worked to reduce vessel damage by limiting inflammation, oxidative stress, and abnormal recycling of energy-producing mitochondria. Oxidative stress occurs when reactive oxygen species (ROS) exceed the ability of antioxidants, including enzymes, to neutralize these toxic oxygen-containing molecules.
According to the researchers, these findings make PRDX2 a promising target for future treatments in people with this rare type of pulmonary hypertension.
“Overexpression [higher levels] of PRDX2 alleviates pulmonary vascular remodeling [structural changes in the blood vessels] in CTEPH,” the team wrote, “suggesting its protective role and potential as a therapeutic target for the disease.”
Their study, “Overexpression of PRDX2 alleviates chronic thromboembolic pulmonary hypertension by modulating inflammation and mitophagy,” was published in the journal Scientific Reports.
CTEPH is caused by long-lasting blood clots that block the pulmonary arteries, which connect the right side of the heart to the lungs. This leads to abnormally high pressure in these blood vessels and forces the heart to work forcefully to pump blood, leading to heart failure.
Still, the researchers noted, the biological underpinnings of CTEPH “are not well understood.”
“There is an urgent need for in-depth studies to clarify its … processes and to provide more effective clinical treatment strategies” for patients, the team wrote.
Scientists use rat model to investigate PRDX2’s role in CTEPH
The researchers found that average PRDX2 levels were significantly higher in the blood of people with CTEPH than in that of healthy individuals. However, the role of this antioxidant enzyme in CTEPH has not been defined.
To explore this, the scientists turned to a preclinical model of CTEPH in which rats are injected with polystyrene microspheres into the bloodstream. These very small, hollow spheres block blood vessels in the lungs, causing high blood pressure.
About three months after injection of the microspheres, average right ventricular systolic pressure or RVSP — a measure of how forcefully the right side of the heart must contract to push blood into the lungs — was significantly higher in model rats than in controls. A separate measure of how well the right side of the heart contracts, known as tricuspid annular plane systolic excursion or TAPSE, was significantly reduced.
When the researchers examined lung tissue under a microscope, they observed marked vascular remodeling in the blood vessels. The walls of the pulmonary arteries were thickened, and there was excessive scarring. PRDX2 was mainly present in the endothelial cells, which line blood vessels. Its levels were significantly higher in the lung tissue of model rats relative to controls, and increased progressively over time.
Inflammatory proteins, such as interleukins and tumor necrosis factor alpha, were also significantly increased in the lung tissue of model rats. Blocking a signaling pathway involved in inflammation with a molecule called BAY-11-7085 significantly reduced levels of those inflammatory proteins. Reducing production of PRDX2 had the opposite effect, suggesting it may be protective.
[The study suggests] PRDX2 as a promising therapeutic target and establishes a basis for further research into the [disease-causing mechanisms] and treatment of CTEPH.
PRDX2 also played a role in mitophagy, which is the process cells use to remove damaged mitochondria, the parts of the cells that produce energy. When levels of PRDX2 were reduced, proteins called LC3II/I and Beclin-1 increased while p62 decreased, showing that mitochondria were being destroyed. Electron microscopy, meanwhile, indicated that many mitochondria were fused with lysosomes, the recycling centers in cells.
In contrast, increasing PRDX2 levels restored these mitophagy markers to normal levels, repaired mitochondria, and reduced ROS. In rats, increasing PRDX2 levels by using a viral vector three weeks before injecting the microspheres improved both RVSP and TAPSE compared with a control (empty) viral vector, while also reducing pulmonary remodeling and death rate.
“These results highlight the protective role of PRDX2,” the researchers wrote.
While the study was done in animals and the model does not replicate all features of the human disease, it suggests “PRDX2 as a promising therapeutic target and establishes a basis for further research into the [disease-causing mechanisms] and treatment of CTEPH,” the researchers concluded.