Blood vessel cells in PAH show cancer-like changes, study finds
Such features in endothelial cells may play role in driving disease
Written by |
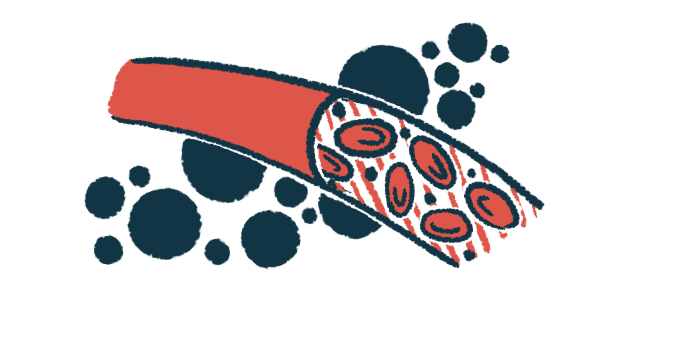
In people with pulmonary hypertension (PH), the endothelial cells that line the inside of blood vessels in the lungs take on features that are similar to what’s seen in some cancers, a new study found.
The researchers who uncovered these features in these hard-to-access cells noted that they may play a role in driving the progressive disease.
“Our findings … provide new evidence of a cancer-like phenotype in [endothelial cells] from the central vasculature of PAH patients,” the researchers wrote, noting that “changes in gene expression [activity] tracked with clinical events in [the] PAH subjects … over time.”
Their study, “Transcriptional profiles of pulmonary artery endothelial cells in pulmonary hypertension,” was published in Scientific Reports.
Study tests new technique allowing endothelial cell collection from patients
PH is defined by increased blood pressure in the vessels that carry blood from the heart through the lungs. A feature of the disease is increased growth of endothelial cells, which regulate exchanges between the blood and surrounding tissues.
While endothelial cell dysfunction is thought to play a central role in driving PH, until recently there has not been a good way to study these difficult-to-access cells in patients.
Now, a team led by researchers at Brown University, in Rhode Island, have developed a technique to isolate and grow endothelial cells that are collected from the tips of balloons used for right heart catheterization — an invasive procedure to measure pressure in the lungs’ blood vessels that’s used to help diagnose and monitor PH.
In this study, the scientists used the technique to analyze endothelial cells from 49 people with pulmonary arterial hypertension (PAH), a rare type of PH. The patients’ median age was 63 and more than two-thirds (69%) were female.
The researchers specifically analyzed the cells’ gene expression profiles, that is, the extent to which individual genes essentially are turned on or turned off in the cell.
Their main goal was to demonstrate that this new method could be used to detect disease-relevant changes in endothelial cell activity — and results in this regard were positive. Specifically, compared with cells from people without PH, endothelial cells from PAH patients showed abnormal expression for more than 600 genes. This included many genes related to biological pathways that previously had been established as being dysregulated in PH. These involved pathways are implicated in processes such as cardiac development, immune cell function, and the production of reactive (toxic) oxygen species.
The scientists found that these changes were consistent over time as the cells were grown in lab. Further, analyses of cells from people with varied clinical presentations showed similar gene expression profiles.
Altogether these data “demonstrated the validity and promise of using [pulmonary artery endothelial cells] cultured from routine [right heart catheterization] balloon tips in living patients with PAH,” the scientists wrote.
The team added that this method “provides an available source of cells that can be repeatedly characterized for deep phenotyping [characterization] over the disease course, a long-standing barrier to translational research in pulmonary vascular disease.” Previously, the team noted, there were “no data from living patients with PAH.”
Some blood vessel cells show resistance to cell death seen in many cancers
While the experiments revealed many changes that were expected for PH endothelial cells, the researchers also noticed something they hadn’t anticipated: Some diseased endothelial cells were resistant to a specific type of cell death.
Under normal circumstances, endothelial cells interact with a mesh of proteins and other molecules called the extracellular matrix, which helps give the tissue its structure. If an endothelial cell becomes detached from its neighbors, it can no longer function properly. Thus, normally, the cell will die in a process called anoikis.
But endothelial cells from PH patients showed resistance to anoikis, the researchers found. The team noted that anoikis resistance hasn’t previously been reported as a major mechanism in PH — but resistance to anoikis has been reported in many types of cancers. Indeed, this is often a critical feature that lets cancer cells metastasize, or spread, throughout the body.
“We provide evidence of anoikis-resistance as a novel paradigm for endothelial proliferation in PAH,” the scientists wrote.
To our knowledge, this ‘cell biopsy’ approach is a first-in-field window into dynamic signatures during the PAH disease course that may be harnessed to refine therapeutic selection.
The team said these findings could potentially aid in the future discovery of new treatment strategies for PAH.
“This ‘cell biopsy’ method may provide insight into patient and lung [endothelial cells] heterogeneity to advance precision medicine approaches in PAH,” the researchers wrote.
“To our knowledge, this ‘cell biopsy’ approach is a first-in-field window into dynamic signatures during the PAH disease course that may be harnessed to refine therapeutic selection,” they concluded.