CAR Peptide Improves Remodulin Efficacy in PH Rat Model
CAR peptide (CAR), Vascular BioSciences’ lead therapeutic peptide candidate for pulmonary hypertension (PH) and other disorders, was found to increase the efficacy of Remodulin (treprostinil) at reducing clinical signs of PH and prolonging the survival of a rat model of the disease.
These preclinical findings were scheduled to be presented in a poster, titled “Cyclic CAR Peptide Modulates the Effects of Treprostinil and Macitentan in Experimental Pulmonary Hypertension,” at the American Thoracic Society’s Annual Meeting. That meeting was cancelled due to the COVID-19 pandemic.
CAR is a small, man-made peptide that naturally targets and penetrates diseased tissues, increasing the effectiveness of other therapies and promoting wound healing.
It is a new form of targeted treatment that is being developed and tested by Vascular Biosciences as an add-on therapy to treat PH and the blood infection sepsis due to its ability to specifically target damaged blood vessels.
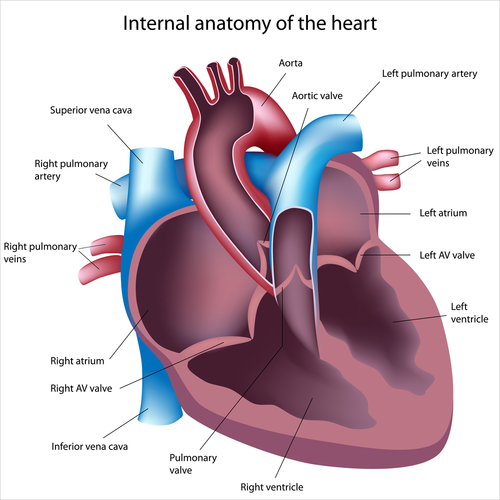
Preclinical data now announced by the company showed that CAR increased Remodulin’s efficacy at lowering blood pressure and reducing abnormal enlargement of the heart’s right ventricle in a rat model of PH. The therapy was given sublingually, meaning it was placed under the tongue, in combination with Remodulin — given as an injection under-the-skin. Remodulin is an approved therapy for pulmonary arterial hypertension (PAH).
Of note, the right heart ventricle is the lower right chamber of the heart that is responsible for pumping blood from the heart into the lungs. In PH patients, the right ventricle may become enlarged and start to malfunction due to the increased blood pressure brought on by the narrowing of blood vessels connecting the heart to the lungs.
Animals receiving the combination therapy also were found to live longer than those receiving Remodulin alone. All (100%) of the animals on the dual treatment survived, compared with 83% of those in the group receiving Remodulin only.
However, when CAR was given alongside Opsumit (macitentan), another approved therapy for PAH, the peptide failed to boost the therapy’s effectiveness at reducing clinical signs of the disease. Nevertheless, animals receiving both therapies also were found to live longer than those receiving Opsumit alone. The findings showed an 85% survival rate with dual therapy around day 50 post-treatment start, compared with 43% in the group receiving Opsumit only.
According to the researchers, these findings indicate that “CAR appears to exert adjuvant [additional] effects that are specific to each class of PH therapy.”
“While further studies are needed to elucidate the mechanisms underlying these selective effects, these findings suggest CAR is potent adjuvant therapy with additive benefit beyond existing PH treatments,” they added.
In another poster prepared for the meeting, the company also showed that CAR — when given intravenously (into the vein) in combination with low-dose hydrocortisone — significantly increased the survival of a rat model of sepsis, compared with hydrocortisone alone.
“Together, these findings demonstrate the unique ability of our CAR peptide to selectively enhance a broad range of therapies and improve survival in preclinical models of both pulmonary hypertension (PH) and sepsis,” David Mann, CEO of Vascular Biosciences, said in a press release.
“Additionally, these results were obtained whether CAR was administered sublingually or intravenously, demonstrating CAR’s unique potential as a pan-therapeutic adjuvant for two very difficult to treat diseases,” Mann said.
According to Mann, CAR’s promising therapeutic potential to treat sepsis — by directing corticosteroids to an injured site — also may be of value in the fight against COVID-19. Both sepsis and septic shock are two main end-stage clinical manifestations of COVID-19 contributing to patient deaths.
“We are hopeful that these findings can be translated to the clinic to help lower the morbidity and mortality of sepsis and COVID-19,” Mann said. “We are working hard to help provide more effective therapies for patients with COVID-19 that develop sepsis, one of its most life-threatening complications,” Mann said.







