Stem cell exosomes may be hypoxic pulmonary hypertension therapy
Researchers use lab-grown cells, rats to better understand disease mechanisms
Exosomes — very small, sac-like structures — derived from stem cells may offer a potential treatment for hypoxic pulmonary hypertension (HPH) by preventing the abnormal growth and movement of muscle cells lining blood vessels.
That’s according to data from a new study, conducted by researchers in China using lab-grown cells and rats, that “suggest a protective effect of [stem-cell]-derived exosomes against HPH.”
“Despite advancements in understanding the pathogenesis [disease development] of HPH, … the incidence and mortality rates of HPH remain high,” the researchers wrote. Thus, “it is crucial to further understand the mechanisms underlying HPH development.”
The study, “Mesenchymal stem cell-derived exosomes improve vascular remodeling by inhibiting EGFR/ErbB2 heterodimerization in hypoxic pulmonary hypertension,” was published in the journal Scientific Reports.
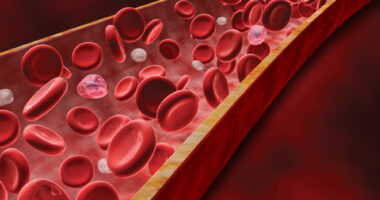
HPH is a disease in which low oxygen causes increased pressure in the pulmonary arteries, which are blood vessels in the lungs. This can result in pulmonary vascular remodeling — abnormal structural changes in the pulmonary arteries, such as thickening of their walls.
Treatment usually involves vasodilators, which reduce pressure by relaxing the smooth muscle around blood vessels. However, these medications aren’t effective for everyone.
According to the researchers, understanding the mechanisms of pulmonary vascular remodeling and HPH could lead to new treatments.
“This understanding can facilitate ongoing research and the development of more effective treatment strategies for HPH,” the team wrote.
Scientists look at using stem cells to repair thickened pulmonary arteries
In this study, the scientists focused on the potential of mesenchymal stem cells — adult stem cells capable of becoming other types of cells — and their exosomes as sources of molecules to repair thickened pulmonary arteries.
Mesenchymal stem cells have anti-inflammatory and tissue repair properties. For their part, exosomes — initially identified as a means of cellular communication — scarcely induce immune responses, which, according to the investigators, “makes them suitable for cell signaling and information exchange.”
“In the context of PH, [mesenchymal stem cell]-derived exosomes improve pulmonary vascular remodeling and reduce pulmonary artery pressure,” the scientists wrote.
Mesenchymal stem cells from bone marrow were grown in the lab. The researchers then collected the fluid where the stem cells were grown and used ultracentrifugation, or essentially very fast spinning, to separate the exosomes. These exosomes measured 50-150 nanometers — about 1,000 times smaller than the width of a human hair — and had a round, dish-like shape.
Pulmonary artery smooth muscle cells (PASMCs) tend to grow excessively in HPH, contributing to the thickening of the pulmonary arteries. To mimic this, the researchers grew PASMCs with PDGFBB, a protein that stimulates their growth. However, when they added the exosomes, the abnormal growth was slowed.
In HPH, these smooth muscle cells also move around excessively. To check if exosomes could reduce this migration, the researchers used a model of wound healing in which they scratched a cell layer and measured how quickly PASMCs filled the gap. Exosomes indeed slowed their movement, the scientists found.
Better understanding ‘crucial’ to hypoxic pulmonary hypertension therapy
The team then turned to an animal model of HPH, exposing rats to low oxygen for eight hours a day over four weeks. These rats had higher right ventricular systolic pressure, which reflects how hard the heart has to pump blood through the lungs, as well as right ventricular hypertrophy, which shows how much the heart muscle thickens.
However, when rats were treated with exosomes, right ventricular systolic pressure and hypertrophy were significantly reduced, indicating their “potential as a therapeutic strategy for attenuating the development of right ventricular hypertrophy and its associated complications in HPH,” which include heart failure, the researchers noted.
To understand how this worked, the team looked at proteins involved in HPH and pulmonary vascular remodeling. They found that two proteins — EGFR and ErbB2 — were elevated in PASMCs exposed to PDGFBB. However, exosomes significantly reduced their levels.
A better understanding of [PHP] … mechanisms is crucial for designing innovative therapies. … Future research will focus on these areas to develop more effective treatments.
Exosomes may work by blocking EGFR and ErbB2 from pairing up — a process called heterodimerization — which seems to be key in preventing the abnormal behavior of PASMCs, according to the team.
“Targeting the EGFR/ErbB2 heterodimer may represent a potential therapeutic strategy for HPH,” the researchers wrote.
Still, more studies are needed, per the team.
“A better understanding of its … mechanisms is crucial for designing innovative therapies for HPH. Future research will focus on these areas to develop more effective treatments,” the researchers wrote.