Israeli Group Pushes for Better Awareness and Treatment of Pulmonary Hypertension
Written by |

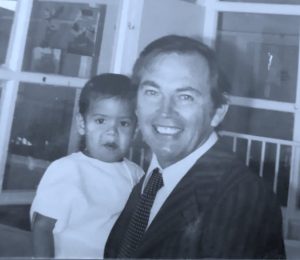
Aryeh Copperman, CEO of the Israel Pulmonary Hypertension Association. (Photo by Larry Luxner)
For two-and-a-half painful years, Jerome Maharaj, 42, had no idea what was wrong with him.
Born in South Africa, he came to Israel in 1996 and settled in Ma’agan, a small kibbutz near the Sea of Galilee. He got married and raised three children.
In early 2016, at the age of 39, he began having serious health problems, notably sharp pains in his stomach. Maharaj consulted his government-appointed family doctor, who told him it could be heart problems — possibly a heart murmur — or asthma.
“But I kept telling him I don’t feel any pain in my chest, upper back or shoulders, that it was something in my stomach, whether I ate or didn’t eat,” said Maharaj, whose oxygen saturation levels had dropped to 83%. “They kept sending me to the same checkups all the time, so I asked to change doctors.”
By March 2018, Maharaj was coughing up blood after any sort of heavy lifting, and realized his situation was urgent.
“I had to threaten them with a lawyer and finally got what I wanted,” he said. Maharaj was examined by the prominent cardiologist Raphael Hirsch at Beilinson Hospital — a unit of Rabin Medical Center — in Petah Tikva, and in August 2018 finally received the proper diagnosis: pulmonary hypertension (PH).
“Dr. Hirsch saved my life,” Maharaj told Pulmonary Hypertension News. “He said, ‘if you didn’t come to me, you could have collapsed and died, without anyone ever knowing what it was.’”
A painful choice
Maharaj’s story is all too familiar, says Aryeh Copperman, CEO of the Israel Pulmonary Hypertension Association (IPHA).
Copperman, interviewed in the Tel Aviv suburb of Ramat Gan, estimates that 600 to 700 of Israel’s 9 million inhabitants have PH — a rare and complex disease characterized by high blood pressure in the lungs.
An accountant by profession and an Orthodox Jew, Copperman became involved with the organization in 2005, when his wife, Rachel, was 33 and pregnant with her fifth child.
“She didn’t have any energy, so she went to a family doctor, who told her it was nothing, that she was stressed and to just calm down and everything would be OK,” Copperman said.
Before long, Rachel couldn’t walk from one room to another without feeling short of breath. Copperman’s father is a cardiologist, and when his daughter-in-law’s symptoms were explained to him, he ordered Copperman to bring Rachel to the hospital immediately. An echocardiogram revealed she had PH.
“They told us we’d have to stop the pregnancy immediately. After three days, nothing changed, so she had an abortion,” said Copperman, adding that he and his wife took the decision after consulting rabbinical authorities, who agreed that it was a necessary lifesaving measure. “Not to finish the pregnancy could have been very dangerous. In our association, we’ve had a few cases where women didn’t want to abort, and one week after giving birth, they died.”
Copperman said his wife remained in the hospital for a month, and that it took her one year to recover to the point where she could travel by car to Jerusalem — a 45-minute trip from their home in the Tel Aviv suburb of B’nei Braq — without having to stop and go outside to breathe.
Increasing awareness in Israel
As a result of her disease, Aryeh, 48, and Rachel, 47, became involved in the Israel PH Association. Within a year, Aryeh Copperman became its chairman, and later on, its full-time CEO. Under his leadership, Copperman said, its annual budget has grown from barely 3,000 shekels (less than $1,000) to around 300,000 shekels (just under $100,000) today.
The IPHA has about 400 registered members and holds an annual conference; the last one took place in May, in the Mediterranean coastal city of Ashkelon.
Copperman said 80% of his association’s members are females — mostly of childbearing age — and that in virtually every case, these women were first told by their physicians that their symptoms were stress-related.
“It’s very hard to know who has PH. You can see it only in an echocardiogram,” he said. “When I went to a physician because I had a pain in my chest, I was immediately sent to the hospital. They did an echo and told me everything was OK and sent me home — but that’s just because I’m a man, not a woman.”
The Israel Pulmonary Hypertension Association is a member of PHA Europe, a Vienna-based nonprofit umbrella group that unites 30 patient associations in 26 countries.
“There’s much more awareness in Israel today,” Copperman said. “The physicians understand a lot more about PH. The hospitals know what you’re talking about. When we started out, nobody knew what PH was.”
Life expectancy has also increased, from two or three years after diagnosis to maybe 20 or 30.
“Patients who are not diagnosed generally die after a year-and-a-half or two years. So it’s very important to be diagnosed as soon as possible,” he said. “These days, the medications are also easier to take — pills instead of IV solutions.”
Portable oxygen concentrators
Copperman’s wife, Rachel, is on several medications. She started with Letairis (ambrisentan) — which is marketed by Gilead in the U.S. and by GlaxoSmithKline in Europe under the brand name Volibris — and is now taking Pfizer’s Revatio (sildenafil) and Uptravi (selexipag), developed by Actelion.
“All these meds help, but they don’t solve the problem,” he said. “Only a lung transplant will cure PH. In Israel, they won’t do lung transplants unless you’ve tried all medications and nothing else helps. But when you do a transplant, it lasts for maybe five years, not more than that.”
He added: “On the other hand, you have to get a transplant before you can no longer do it.”
The organization hosts frequent PH “awareness days” at shopping malls across the country, and has made several rather moving videos — examples are here and here — highlighting what it’s like to live with the disease.
In addition, the IPHA has made available to its members about 40 battery-powered portable oxygen concentrators, costing the equivalent of $5,000 each. The machines enable patients who need oxygen to leave their homes.
“In the States, they rent these machines for $200 a week, and we rent them out for $80 a month,” Copperman said. “We give them all over Israel to patients — not just those with PH but also cystic fibrosis, cancer patients, and others. We are the only organization in the world I know of that does this.”
PH patients in Israel are treated at five specialized clinics: Tel Hashomer in the Tel Aviv metro area, Beilinson in Petah Tikva, Hadassah Ein Kerem in Jerusalem, Carmel in Haifa, and Soroka in Beersheva. The Soroka clinic, in particular, serves Bedouin Arabs living in the Negev Desert and elsewhere throughout southern Israel.
PH: A daily struggle
Maharaj, the South African-born PH patient who had to threaten a lawsuit to see the doctor of his choice, has not yet had a lung transplant. But surgery isn’t exactly new to him.
As a 2-year-old, Maharaj had surgery for transposition of the great arteries; the doctor who operated on him was Cape Town cardiologist Christiaan Barnard, who 12 years earlier achieved worldwide fame for performing the world’s first human heart transplant.
“Here in Israel, not too many doctors — even lung doctors — know about PH. They thought that because of my constant coughing it was a problem of reflexes in my esophagus. It’s quite sad that even pulmonologists don’t have the experience to think of PH.”
Maharaj inhales Ventavis (iloprost) — a solution marketed in Israel and the EU by Bayer — five times a day using the I-neb inhaler, and takes at least four other medications to control PH-related symptoms.
Because he lives in a flat area, Maharaj can walk his two dogs twice a day; that’s his exercise. Since getting his diagnosis, he said that his “life has changed drastically” — and not for the better.
“The things I used to do with my kids, I can’t do anymore. My son asks me to play football, but I can’t. I kick the ball a few times and I have to stop,” Maharaj said, adding that he avoids “food that are too sweet, too acidic or too salty” because they give him stomach pains.
“I have to watch my emotions. Laughing or crying has an effect on me and can be very difficult,” he said. “I can’t even do desk work anymore, because if I sit for too long, I start getting spasms in my legs, and the pain goes up to my lower back. I live in a two-story house and the bedrooms are upstairs. Every time I climb the 20 steps, I’ve got to think what to take with me.”