Low circALMS1 levels could be prognostic biomarker in PH: Study
Low protein levels promote higher numbers, migration of PMECs
Written by |
Low levels of circular RNA Alstrom syndrome protein 1, or circALMS1, may be associated with poor outcomes with pulmonary hypertension (PH), a study suggests.
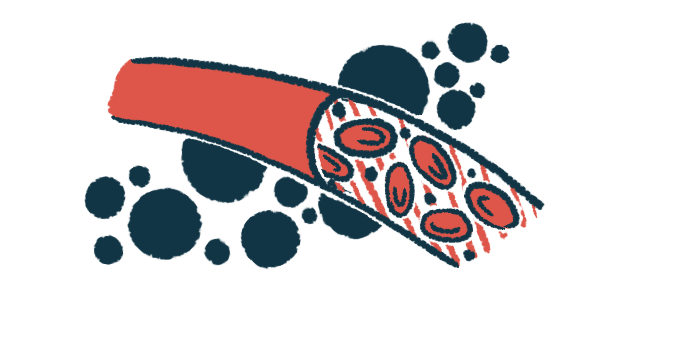
This may be because low circALMS1 levels promote higher numbers and the migration of pulmonary microvascular endothelial cells (PMECs), and reduce the cells’ death. PMECs line the walls of small blood vessels and may factor in lung arteries’ lesions in PH. This may make circALMS1 a promising diagnostic and prognostic indicator in PH, say researchers in “CircALMS1 Alleviates Pulmonary Microvascular Endothelial Cell Dysfunction in Pulmonary Hypertension,” which was published in the Journal of the American Heart Association.
“Our study provided relevant and novel data to understand the underlying mechanisms of pulmonary vascular remodeling, which could lead to the development of new therapeutic targets for PH,” they wrote.
A feature of PH is high blood pressure in the pulmonary arteries, the blood vessels that supply the lungs, and is associated with the dysfunction of endothelial cells, which line the walls of blood vessels. Increased blood pressure in the lungs makes the right side of the heart work harder to pump blood. Under adverse conditions, such as low oxygen levels, or hypoxia, PMECs in small vessels multiply, leading to plexiform lesions.
Circular RNAs, a type of molecule thought to control the activity of certain genes, can influence PH’s development. In fact, a growing number of studies suggest these molecules may be biomarkers for the diagnosis, prognosis, and treatment of vascular diseases.
Uncovering function of circular RNAs in PH
“However, their function in pulmonary vascular intimal injury remains undefined,” wrote researchers in China, who sought to identify circular RNAs specifically expressed in PMECs in the context of hypoxia and PH. The tunica intima is the innermost and thinnest endothelial cell layer.
The researchers started by growing PMECs in the lab and exposing them to hypoxia or normal oxygen conditions, using sequencing analysis to identify all the differentially expressed genes.
They identified 86 circRNAs at higher levels, or upregulated, in PMECs that were exposed to low oxygen, while 41 — including circALMS1 — were reduced, or downregulated.
Then they analyzed the expression of circALMS1 in blood samples of 69 PH patients — 33 with idiopathic, or no known cause, pulmonary arterial hypertension and 36 with PH caused by chronic obstructive pulmonary disease — and 69 healthy participants.
Results showed circALMS1 was significantly downregulated in PH patients compared with healthy people, and lower levels of the molecule were associated with a significantly higher risk of death.
Levels of circALMS1 were then increased in two rat models of PH by using a viral vector containing the genetic sequence that codes for this circular RNA molecule. This resulted in less pulmonary arterial remodeling (structural alterations) and improved right heart function.
Higher circALMS1 inhibited the growth and migration of lab-grown PMECs and promoted their death under hypoxic conditions. Important for this effect was the interaction between circALMS1 and a micro RNA molecule named miR‐17‐3p and that of miR‐17‐3p with its target gene YTHDF2. Micro RNAs are small RNA molecules that regulate protein production.
YTHDF2 protein levels were reduced in hypoxic PMECs, which was associated with an increase in PMECs growth and migration along with lower cell death. “The results indicated that, although YTHDF2 … contributes to the degradation of many circular RNAs, it could not regulate the circALMS1 levels in PMECs,” wrote the scientists, who said “circALMS1 worked as an miR‐17‐3p sponge to regulate YTHDF2 expression, promoting proliferation, migration, and reducing apoptosis of PMECs under risk factors.” Apoptosis is a type of programmed cell death, as opposed to death caused by injury.
“Our study sheds new light on circALMS1‐regulated dysfunction of PMECs by the miR‐17‐3p/YTHDF2 pathway under hypoxia and provides insights into the underlying pathogenesis [disease processes] of PH,” they said.