Balloon Angioplasty Aids CTEPH Patients, But in Ways That May Depend on Lung Area Treated
The specific benefits of balloon pulmonary angioplasty (BPA) on the respiratory function of patients with chronic thromboembolic pulmonary hypertension (CTEPH) depends on what area of the lung, or lung field, the procedure is performed on, according to new research.
This finding was published in the article “Effect Of Balloon Pulmonary Angioplasty On Respiratory Function In Patients With Chronic Thromboembolic Pulmonary Hypertension” in the journal CHEST.
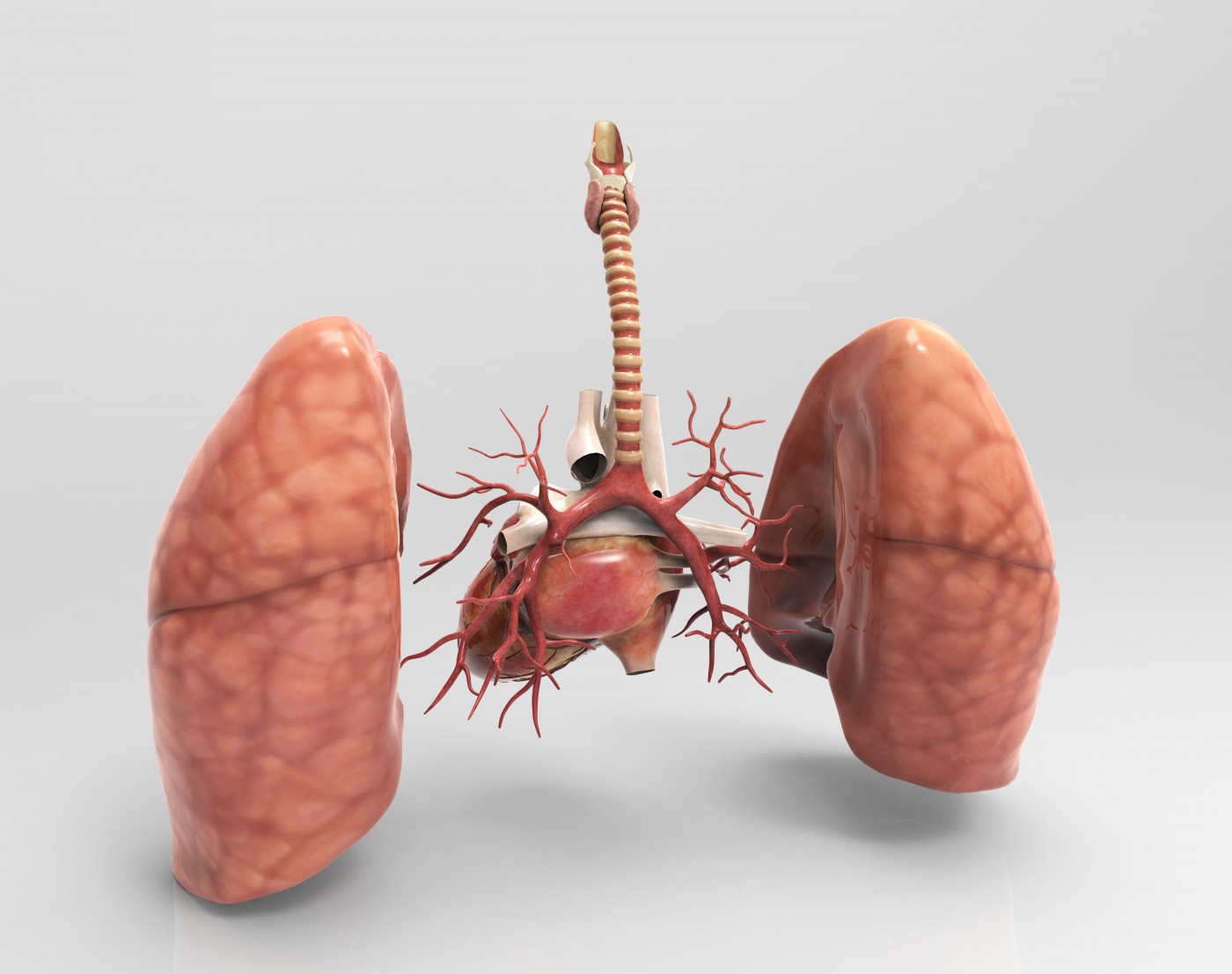
CTEPH, which results from chronic obstruction of large and small pulmonary arteries, is most often treated by pulmonary endarterectomy (PEA), an operation to remove blood clots. But a considerable proportion of patients (37 percent) are not able to undergo this surgery.
BPA has emerged as a treatment option for these patients, and been shown to improve pulmonary hemodynamics and long-term outcomes. In this procedure, a long thin tube is placed in the constricted artery and then inflated during surgery to increase the width of the blood vessel, which improves blood flow.
“Recently, balloon pulmonary angioplasty (BPA) has been reported to improve hemodynamics and functional capacity in patients with chronic thromboembolic pulmonary hypertension (CTEPH) who are not candidates for pulmonary endarterectomy,” Mina Akizuki, the study’s lead author, said in a news release. “However, BPA effect on respiratory functions is unclear.”
Akizuki and colleagues followed 13 patients with inoperable CTEPH, who underwent BPA in arteries of either the lower lung lobes or those of the upper and middle lobes. The team investigated the effect of 62 BPA sessions on hemodynamics, ventilator efficiency, and gas exchange using right heart catheterization, a respiratory function test, and cardiopulmonary exercise testing (CPX). Results were compared and analyzed against the different BPA lung fields treated.
BPA, overall, improved the mean pulmonary artery pressure (44 to 23 mmHg) and pulmonary vasculature resistance (818 to 311 dyne/s/cm-5), the researchers reported.
But in patients who underwent BPA in the lower-lung field, the percentage of predicted carbon monoxide lung diffusion capacity (%DLco, a measure of gas exchange) decreased (from 60 to 54 percent), with no recovery. In contrast, the %DLco increased for patients who had BPA in the upper-middle lung field (from 53 to 58 percent), and continued to improve during follow-up (from 58 to 64 percent).
Moreover, the VE/VCO2 slope (a measure of ventilator efficacy; increased values indicate a higher risk of cardiac complications) significantly improved in patients after BPA in the lower-lung field (from 51 to 41) and continued to improve during follow-up (from 41 to 35). In those who underwent BPA in the upper-middle lung field, this measure remained unaltered.
These findings showed that both measures of respiratory function — %DLco and VE/VCO2 slope — differed significantly depending on whether an intervention was to the lower or to upper-middle lung fields.
“Based on our results, we suggest that BPA in the lower lung field improves oxygenation and respiratory function parameters during exercise, such as VE/VCO2 slope, because of remarkable improvement in hemodynamics,” the researchers wrote. “BPA in the upper-middle lung field may improve oxygenation and respiratory function parameters at rest, such as %DLco.”







