Balloon Angioplasty Seen to Benefit People with Inoperable CTEPH and Other Conditions, Too
Written by |
Balloon pulmonary angioplasty (BPA) appears to be of multiple benefit to patients with chronic thromboembolic pulmonary hypertension (CTEPH), both in terms of hemodynamics and in other systemic disorders like glycemic control and kidney disease, according to a study published in the journal Circulation, titled “Multiple Beneficial Effects of Balloon Pulmonary Angioplasty in Patients With Chronic Thromboembolic Pulmonary Hypertension.”
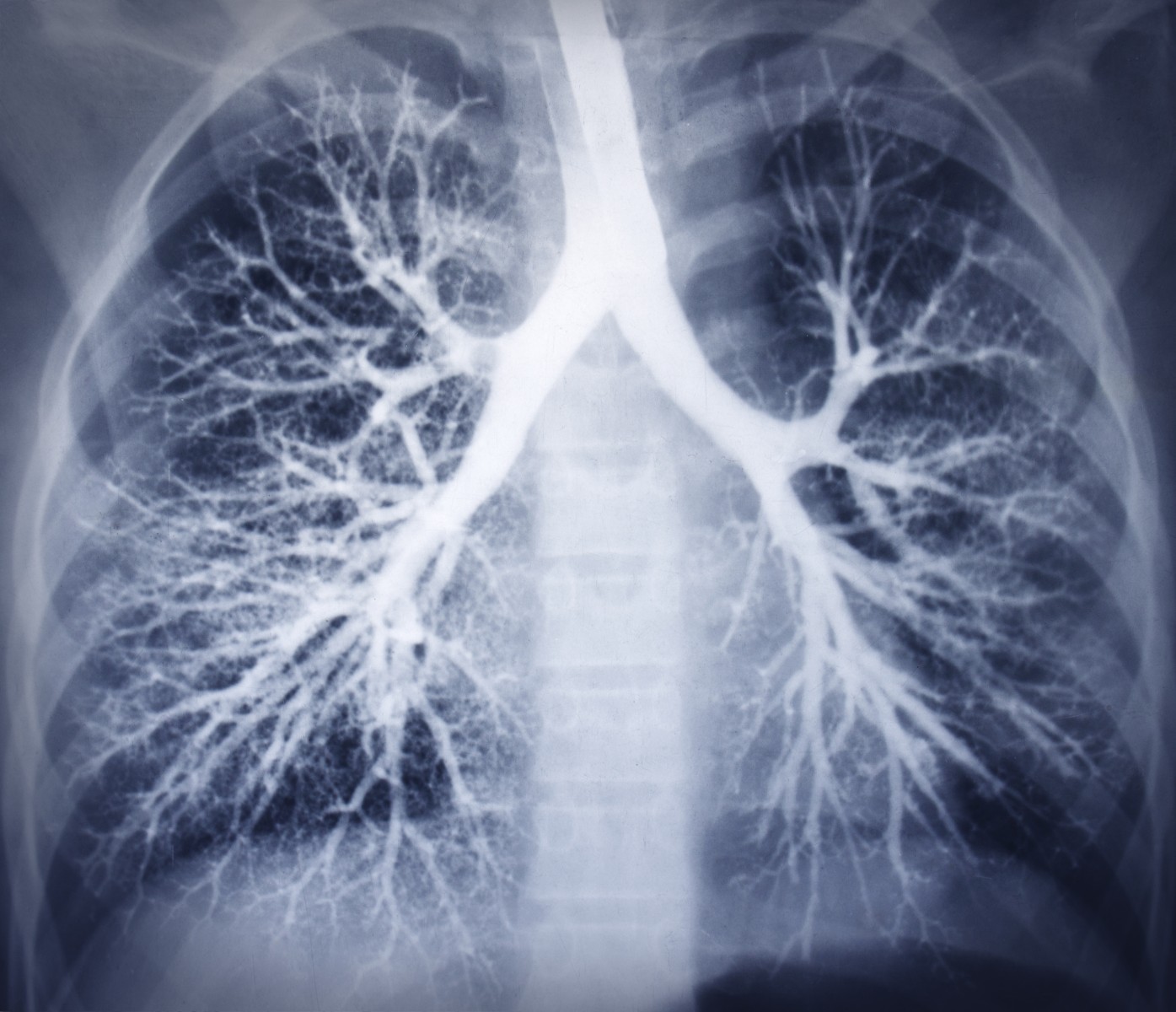
CTEPH is characterized by chronic and mechanical thromboembolic obstruction of large and small pulmonary arteries, requiring intervention. Although pulmonary endarterectomy (PEA) is recommended for the treatment of CTEPH, 37 percent of the cases are considered inoperable. Recent evidence has shown that balloon pulmonary angioplasty (BPA), a new catheter-based treatment option for patients with inoperable CTEPH, markedly improves the pulmonary hemodynamics and the long-term prognosis in patients.
Pulmonary arterial hypertension with systemic dysfunctions, including metabolic disorders and renal dysfunction, has a poor prognosis.
Shunsuke Tatebe, MD, PhD, from the Department of Internal Medicine, Division of Cardio-Vascular Medicine, Kurume University School of Medicine in Japan, and colleagues examined whether CTEPH is associated with systemic dysfunctions in proportion to the severity of the disorder and, if so, whether BPA could improve systemic dysfunctions as well as hemodynamics in CTEPH patients.
A total of 55 people who underwent BPA for systemic dysfunctions were assessed for nutritional status, glycemic control, lipid profiles, and renal and vascular function. The analyses were conducted before and after BPA. Changes in hemodynamic parameters were compared.
Baseline prevalence of hypertension, diabetes mellitus, dyslipidemia, and advanced chronic kidney disease in patients was found to be, respectively, 58 percent, 7 percent, 33 percent and 36 percent. BPA resulted in hemodynamic improvements in the patients, as well as improved nutritional status, dysglycemia, and renal and vascular functions. Notably, the degrees of the hemodynamic improvements were positively correlated with those of other improvements.
According to the researchers, the study “demonstrated that CTEPH significantly improves WHO functional class, exercise capacity, and pulmonary hemodynamics in patients with inoperable CTEPH.”
“BPA decreases right ventricular afterload by eliminating obstructions of small pulmonary arteries (…) End-organ functional improvements could be achieved by increased organ perfusion and decreased organ venous congestion. However, some improvements in systemic dysfunction were associated with improvements in functional and exercise parameters, but not with those in hemodynamics. Thus, improvements in heart failure symptoms after BPA may also be related with improvements in systemic dysfunctions,” the researchers concluded.



