People with severe CTEPH see improved risk profile with treprostinil
81 study participants were randomized to receive high, low dose of therapy
Written by |
Treatment with treprostinil improved the risk profile in people with inoperable or persistent severe chronic thromboembolic pulmonary hypertension (CTEPH).
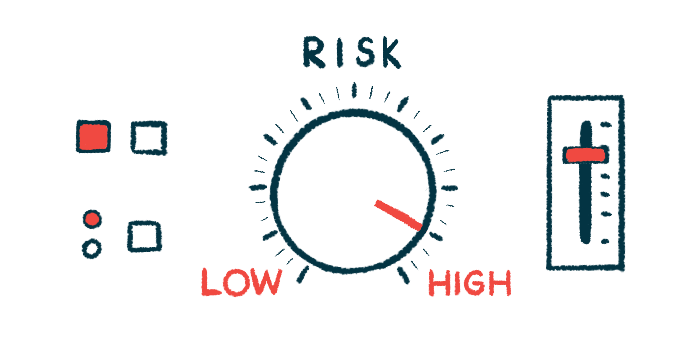
The risk profile was assessed using a risk score established to predict a response to treatment and survival in people with pulmonary arterial hypertension (PAH), the most common type of pulmonary hypertension.
The “assessment of risk profile is of great importance to this particular patient population with very poor prognosis,” the researchers wrote in “The risk profile change in patients with severe chronic thromboembolic pulmonary hypertension treated with subcutaneous treprostinil,” which was published in Pulmonary Circulation.
CTEPH is a form of pulmonary hypertension — high blood pressure in the vessels of the lungs — caused by blood clots that obstruct the lung arteries. The blood clots usually travel from deep veins in the legs or other parts of the body and restrict blood flow to the lungs, leading to increased blood pressure and reduced oxygen reaching the body.
The mainstay and potentially curative treatment for CTEPH is pulmonary endarterectomy (PEA), or surgery to remove blood clots from the pulmonary arteries. Up to half the patients can’t have the surgery, however, and in up to a quarter PH persists or recurs.
Testing risk profile in CTEPH
For these patients, treatment options include using a balloon to open blood vessels (a procedure called balloon pulmonary angioplasty) and medications such as treprostinil (sold as Remodulin, among others) and Adempas (riociguat). Evaluating a patient’s risk might contribute to selecting optimal treatment with respect to medications.
However, “to date, there is no established scoring system for risk stratification specific for CTEPH,” the researchers wrote.
The Registry to Evaluate Early and Long‐Term Pulmonary Arterial Hypertension Disease Management risk score (RRS) was developed in the REVEAL Registry (NCT00370214) to predict survival with pulmonary arterial hypertension. It can also assess the risk and treatment response with CTEPH.
The score evaluates a patient’s risk based on several parameters, including age and gender, kidney insufficiency, blood pressure, heart rate, World Health Organization (WHO) functional scale, 6 minute-walk distance, the resistance in pulmonary vessels, and N-terminal pro-brain natriuretic peptide (a measure useful in diagnosing heart failure).
A team led by Czech Republic researchers used RRS in patients who enrolled in the Phase 3 CTREPH trial (NCT01416636), which is assessing the effectiveness and tolerability of administering treprostinil subcutaneously (under the skin) in adults with inoperable or persistent CTEPH over 24 weeks.
Of 81 participants, 40 were randomized to receive high-dose treprostinil (target dose around 30 nanograms (ng)/kg/min) and 41 to a low-dose treprostinil (target dose around 3 ng/kg/min). The low dose is not used in real-life clinical practice and was intended as a control that can cause the same site reactions to the therapy’s administration.
The patients’ mean age was 64 and most were men (57%). At the study’s beginning (baseline), the mean RRS was similar between the two groups — 8.7 in the high dose and 8.6 in the low dose — which classified them as high risk (RSS scores higher than 8 are considered high risk).
The mean change between baseline and week 24 (around six months) was significantly higher in the high-dose group than the low-dose group (– 0.88 vs. – 0.17). Moreover, more than half the patients (55%) in the high-dose group improved their RRS score after 24 weeks on treprostinil compared to about a third (34%) in the low-dose group. Plus, 17.5% of high-dose patients saw their risk worsen, compared to 27% of low-dose patients. The extent of RRS improvement was not dependent on the risk severity at baseline.
The researchers also analyzed the parameters used to calculate RRS to further evaluate the main factors leading to RRS improvement. The difference between high- and low-dose groups was mainly attributable to WHO functional scale (50%) and NT-BNP (32%), they observed.
“WHO functional class and NT-BNP again showed the greatest difference of the mean change of points from baseline to week 24 between high-dose and low-dose arms,” the researchers wrote.
The study shows a significant improvement of risk score after administering standard doses of treprostinil in patients with severe inoperable or persistent CTEPH. The relatively low number of patients, which didn’t allow the use of a more complex analysis to assess detailed information on risk assessment and survival, and using a risk score for PAH patients were noted as limitations of the study. The researchers said future research should focus on the “main drivers of survival in patients with severe CTEPH” and identifying treatment targets for improving long-term outcomes.