Chronic Thromboembolic Pulmonary Hypertension Patients Still Benefit Six Months After Balloon Angioplasty
Balloon pulmonary angioplasty, a procedure to widen narrowed lung blood vessels, was still benefitting patients with chronic thromboembolic pulmonary hypertension (CTEPH) six months after doctors performed it, a Japanese study found.
The procedure increased patients’ cardiac output, or amount of the blood the heart is pumping, and exercise capacity, researchers said.
The study, “Midterm Effect of Balloon Pulmonary Angioplasty on Hemodynamics and Subclinical Myocardial Damage in Chronic Thromboembolic Pulmonary Hypertension,” was published in the Canadian Journal of Cardiology.
The research included 67 CTEPH patients who had angioplasty between November 2012 and January 2016.
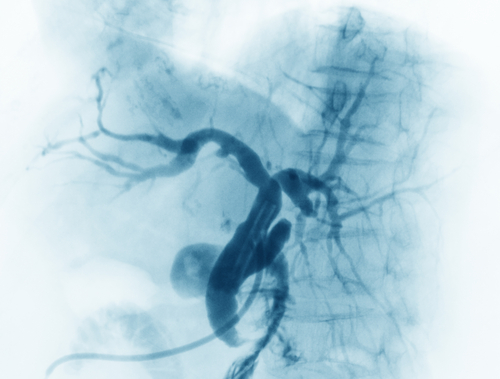
Angioplasty involves inserting a tiny inflatable balloon into blood vessels that supply the lung — vessels that are narrowed in CTEPH. Doctors guide the balloon with a wire. Both are inserted into a vein in the groin or neck. The balloon inflates when it reaches the parts of pulmonary blood vessels that are narrow.
Researchers measured pulmonary artery pressure and pulmonary vascular resistance to evaluate hypertension in lung blood vessels. They took the measurements before angioplasty, a week later, and at six months. Both measures improved, and the improvement lasted six months in most of the patients tested.
Researchers also discovered that cardiac output increased after angioplasty, and was maintained.
Patients were also evaluated for two biomarkers of heart damage: B-type natriuretic peptide (BNP) and high sensitivity troponin T (hs-TnT). The measurements of both biomarkers improved.
But the greatest improvement in hs-TnT was in patients whose heart function was poorer to begin with and who required more angioplasty sessions than the others. The same was seen with cardiac output.
Exercise capacity was measured with the six-minute walking distance (6MWD) test. The average distance patients were able to walk rose from 322 meters before angioplasty to 446 six months after treatment.
Six months after angioplasty, “hemodynamics [blood flow] and exercise capacity improved and hs-TnT levels decreased,” the researchers said. “Improvements in CO [cardiac output] and hs-TnT levels were more prominent in CTEPH patients with impaired baseline hemodynamics. This suggested that angioplasty “has a favorable mid-term effect on hemodynamics and subclinical myocardial damage in patients with CTEPH, especially in those with impaired hemodynamics,” the team concluded.







