Researchers Study PAH in Rheumatoid Arthritis Versus Idiopathic PAH
Written by |
 A new study out of Toronto, Canada has evaluated whether rheumatoid arthritis-associated pulmonary arterial hypertension (RA-PAH) is a more severe disease compared to idiopathic pulmonary arterial hypertension (IPAH). Published on January 13, 2015, the study is titled “Survival in rheumatoid arthritis-associated pulmonary arterial hypertension compared with idiopathic pulmonary arterial hypertension” and appeared in the journal Respirology.
A new study out of Toronto, Canada has evaluated whether rheumatoid arthritis-associated pulmonary arterial hypertension (RA-PAH) is a more severe disease compared to idiopathic pulmonary arterial hypertension (IPAH). Published on January 13, 2015, the study is titled “Survival in rheumatoid arthritis-associated pulmonary arterial hypertension compared with idiopathic pulmonary arterial hypertension” and appeared in the journal Respirology.
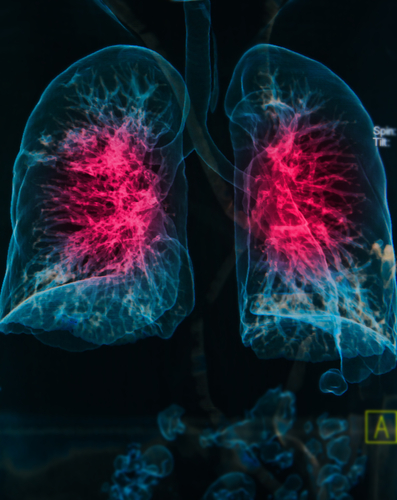
Pulmonary arteries enable the flow of blood from the heart to the lungs, where the blood picks up oxygen for the body. In pulmonary arterial hypertension (PAH), the pulmonary arteries contract, forcing the heart to work faster and causing high blood pressure (hypertension).
[adrotate group=”4″]
PAH refers to high blood pressure of the lungs. It can be associated with different diseases, such as arthritis, or can be of unknown cause (idiopathic). According to the American Lung Association, “PAH worsens over time and is life-threatening because the pressure in a patient’s pulmonary arteries rises to dangerously high levels, putting a strain on the heart. There is no cure for PAH, but several medications are available to treat symptoms.”
The researchers studied RA-PAH and IPAH by retroactively reviewing data that had been collected by the University Health Network Pulmonary Hypertension Programme in Toronto, Canada. Their main goal was to measure mortality (death) due to either of the diseases, using a statistical analysis.
[adrotate group=”3″]
The scientists screened over 1,385 patients and identified 18 people with RA-PAH and 155 people with IPAH. The RA-PAH patients were of older median age at the onset of the disease, with a typical age of 64, compared to about 54 in the IPAH group. The RA-PAH group also had lower average pulmonary arterial pressure (mPAP). More RA-PAH were female, 83% compared to 70% of the IPAH group. However, the RA-PAH did better on a test of walking than the IPAH group. A total of 35 deaths occurred in all of the individuals studied. Of these, 2/18 (11%) were RA-PAH patients and 33/155 (21%) were IPAH patients. However, a statistical test estimating 1-year survival was comparable for the two groups, at 93% for RA-PAH and 94% for IPAH, respectively.
In their report, the researchers concluded that, “Compared with IPAH patients, RA-PAH patients have an older age of onset and lower baseline mPAP. RA-PAH patients have comparable survival to IPAH patients.”
It seems that regardless of the cause of pulmonary arterial hypertension, the rate of survival following the diagnosis remains consistent. Understanding the characteristics of these two types of pulmonary hypertension may help direct treatment, and may also assist in the prediction of the progression of these diseases.



