Vagus Nerve Found To Regulate Pulmonary Fibrosis Progression
Written by |
In a new study entitled “Vagotomy attenuates bleomycin-induced pulmonary fibrosis in mice,” researchers investigated the role of the vagus nerve in pulmonary fibrosis pathogenesis. They established a mouse model and discovered that the vagus nerve regulates pulmonary fibrosis progression by controlling pro-fibrotic factors. The study was published in the journal Scientific Reports.
Pulmonary fibrosis (PF) progression occurs as a result of complex interactions of immune and non-immune factors, including several different types of cells (fibroblasts, myofibroblasts, macrophages, T helper-2) and cytokines (small secreted proteins released by immune cells regulating interactions and communication between cells), particularly the transforming growth factor β (TGF-β) and interleukin 4 (IL-4). The disease is characterized by scarring of the lung tissue. However, in most cases the underlying trigger for PF remains unknown.
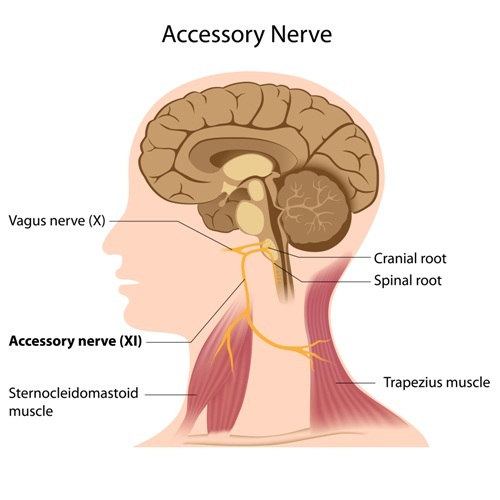
Recent studies suggested that the vagus nerve plays a key role in regulating the release of cytokines, several of which play a role in promoting fibrosis. However, its function in PF is currently unknown. The longest of the cranial nerves, the vaugus nerve (also known as cranial nerve X) extends from the base of the brain (brainstem) to the abdomen, interacting with multiple organs including the heart, esophagus and lungs.
With reports suggesting that stimulating the vagus nerve increases the fibrogenic cytokines in humans, such as TGF-β, the study authors hypothesized that activation of the vagus nerve promotes the disease and vagotomy should attenuate PF (vagotomy is a surgical procedure that involves removing part of or resection of the vagus nerve).
To test their hypothesis, authors assessed and compared the extent and severity of fibrosis in bleomycin-induced fibrosis lungs with and without vagal innervation in the same mouse (bleomycin-induced fibrosis is the most frequently used rodent model of lung fibrosis, producing an inflammatory and fibrotic profile similar to the human pulmonary fibrosis; bleomycin administration leads to the accumulation of white blood cells – particularly macrophages – and activates fibroblasts inducing the deposition of collagen).
They found that indeed the vagus nerve influences bleomycin-induced PF. Specifically, the team observed that vagotomy decreased collagen deposition; attenuated structural destruction; reduced the synthesis of pro-fibrogenic cytokines and suppressed pro-fibrogenic cells.
In summary, the authors established a mouse model that enabled to investigate the role of the vagus nerve in the development of PF and found the vagus nerve action regulates PF progression by controlling fibrogenic-producing cells and cytokines.



