HDL component ApoA-I predicts mortality in PAH: Study
Patients have lower levels of 'good cholesterol'
Lower levels of apolipoprotein A-I (ApoA-I), a component of high-density lipoprotein (HDL), or “good cholesterol,” is a significant predictor of mortality in people with pulmonary arterial hypertension (PAH), a study suggests.
“Our study identified the significance of ApoA-I as a biomarker for predicting the survival outcome of PAH patients,” wrote researchers in “Impact of reduced apolipoprotein A-I levels on pulmonary arterial hypertension,” which was published in the Hellenic Journal of Cardiology.
In PAH, the small arteries where blood is transported from the heart to the lungs narrow, leading to high blood pressure, right heart dysfunction, and an increased mortality risk.
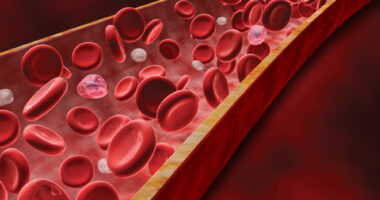
People with PAH have an abnormal lipid (fat) profile in their bloodstream. In particular, PAH patients have lower levels of HDL, a protein complex that transports lipids such as cholesterol throughout the blood.
ApoA-I is a component of HDL with anti-inflammatory properties, and reduced levels have been associated with worse outcomes in pulmonary hypertension, leading researchers in China to explore ApoA-I’s role in PAH and see if it can predict disease outcomes.
ApoA-I’s association with mortality in PAH
First, they measured overall protein production (proteomics) in the lung tissue of six PAH patients, ages 16-38, and four control lung donors, who had all undergone a lung transplant.
Lung tissue from PAH had 168 proteins associated with lipid metabolism that were differentially expressed, or produced at different levels, compared to controls. ApoA-I was identified as an essential protein associated with PAH through a protein-protein interaction analysis.
The researchers then measured several lipid-related molecules in blood samples from 343 PAH patients, who had a mean age of about 40, 246 (71.7%) of whom were women. A group of 266 age-matched healthy people served as controls.
PAH patients had significantly lower levels of ApoA-I, HDL, total cholesterol, and apolipoprotein E, another protein component of HDL, than the healthy people. Significantly higher levels of triglycerides (fat), low-density lipoprotein (LDL), or “bad cholesterol,” and apolipoprotein B, a component of LDL, were found in PAH samples over the controls.
Statistical calculations revealed that lower total cholesterol, HDL, and ApoA-I, and higher triglycerides, were all independent risk factors for PAH. ApoA-I and HDL were significantly associated with reduced survival.
Survival rates
Among those with low ApoA-I, the one-year survival rate was 92.2%. After two years it was 81.0% and it was 69.8% after three years. Likewise, low-level HDL was associated with an 88.4% survival rate after one year, 83.3% after two years, and 70.5% after three years. ApoA-I was better at predicting mortality than HDL, overall.
The optimal cutoff value of ApoA-I was determined to be 1.085 grams per liter of blood. During a follow-up period of 41 months (3.4 years), 92 PAH patients died. Those with ApoA-I levels below the cutoff were significantly associated with worse outcomes.
ApoA-I production was also significantly lower in the lung tissues of a PAH rat model than in those of control rats.
The researchers then measured the levels of various immune signaling proteins associated with inflammation. Of these, only interleukin-6 (IL-6) was significantly related to PAH risk. Although no relationship was found between IL-6 and high or low levels of HDL, elevated IL-6 was more common in patients with ApoA-I below the cutoff value.
In human cell-based tests, IL-6 significantly enhanced the growth of cells that line blood vessels called endothelial cells, whose dysfunction is a major player in arterial narrowing in PAH.
Under normal oxygen conditions, treatment with HDL or ApoA-I significantly alleviated the excess growth of endothelial cells exposed to IL-6. Also, small doses of HDL and ApoA-I significantly suppressed the release of IL-6 from immune cells called macrophages.
“HDL-related proteins were significantly downregulated [lower] in patients with PAH,” the researchers said. Tissue analysis found “ApoA-I to be a key protein among the differentially expressed proteins in the lung tissue of patients with PAH.”
“ApoA-I and HDL-C were found to be potential predictors of prognosis in patients with PAH,” the researchers added, with ApoA-I exhibiting “greater advantages compared with HDL-C for predicting the risk of death.” Larger scale prospective studies at multiple centers with long-term follow-up are needed to validate the study, the researchers said.