Echocardiograms Can Help Identify PAH Patients at High Risk of Death, Study Reports
Written by |
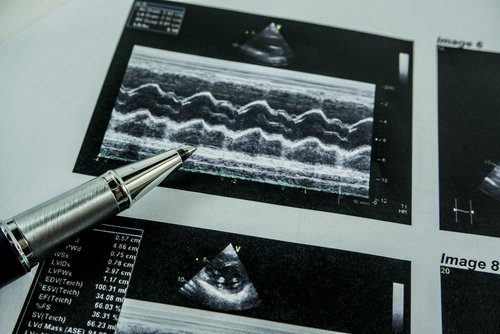
High blood pressure in the right artery makes a person with pulmonary arterial hypertension almost 2 1/2 times more likely to die than a patient with lower pressure, according to a study focusing on how doctors can use echocardiograms to predict poor PAH prognosis.
Other echocardiogram measurements that can signal poor outcome are a leaking tricuspid valve and accumulation of fluids around the heart. The tricuspid valve prevents deoxygenated blood from flowing backward from the right atrium of the heart to the right ventricle. If it’s leaking, blood does flow backward, disrupting flow to other parts of the heart.
The point of the article in the American Heart Journal is that some electrocardiogram measurements can help doctors spot patients at high risk of a poor PH prognosis. As the researchers put it, “The identification of high-risk echocardiographic features may provide an opportunity for timely and enhanced PAH therapy.”
The research was titled “High-Risk Echocardiographic Features Predict Mortality in Pulmonary Arterial Hypertension.”
After a diagnosis, doctors at expert PAH centers need to monitor patients closely to ensure suitable care and prevent or delay the disease’s progression. Although doctors order biomarker and other tests to gain a grasp of a person’s disease, they haven’t had a reliable tool to predict outcome.
Early identification and treatment of PAH is paramount because the disease is life-threatening. Advances in treatment have improved patient survival rates, but doctors have needed a way to identify those at risk of a poorer prognosis.
Some echocardiogram measurements have suggested an increased risk of PAH patients dying, according to previous research. Those studies have included patients in the Registry to Evaluate Early and Long-term PAH Disease Management, or REVEAL.
Researchers decided to do a comprehensive analysis of the PAH prognostic potential of echocardiogram measurements. The study covered 175 patients with Group 1 PAH at the Mayo Clinic Florida in Jacksonville.
Researchers used echocardiograms to assess patients’ heart function. They found that the risk of death among those with high right atrium blood pressure was 2.4 times higher than those with lower pressure. They also discovered that moderate to severe tricuspid valve leaking and accumulation of fluids around the heart were other predictors of poor patient outcomes.
The team validated their findings in a group of 677 patients. The presence of all three risk factors made it five times more likely that a PAH patient would die within a year, compared with those without the factors, the researchers found. Another finding was that the factors made it 3.4 times more likely a patient would die within three years.
“The presence of these high-risk echocardiographic parameters correlated” with PAH severity measures, the researchers wrote. In addition, they showed “similar diagnostic utility” as the risk scores in the REVEAL research, they wrote.
Their study supported the notion that echocardiogram measurements can be reliable sources of prognostic information for PAH physicians.
Long-term studies on “the clinical role of these high-risk ECHO features is warranted, as it may aid in diagnostic and prognostic decision-making,” the team concluded.



