How Advanced Lung Cancer Might Lead to PAH Traced in Study
Written by |
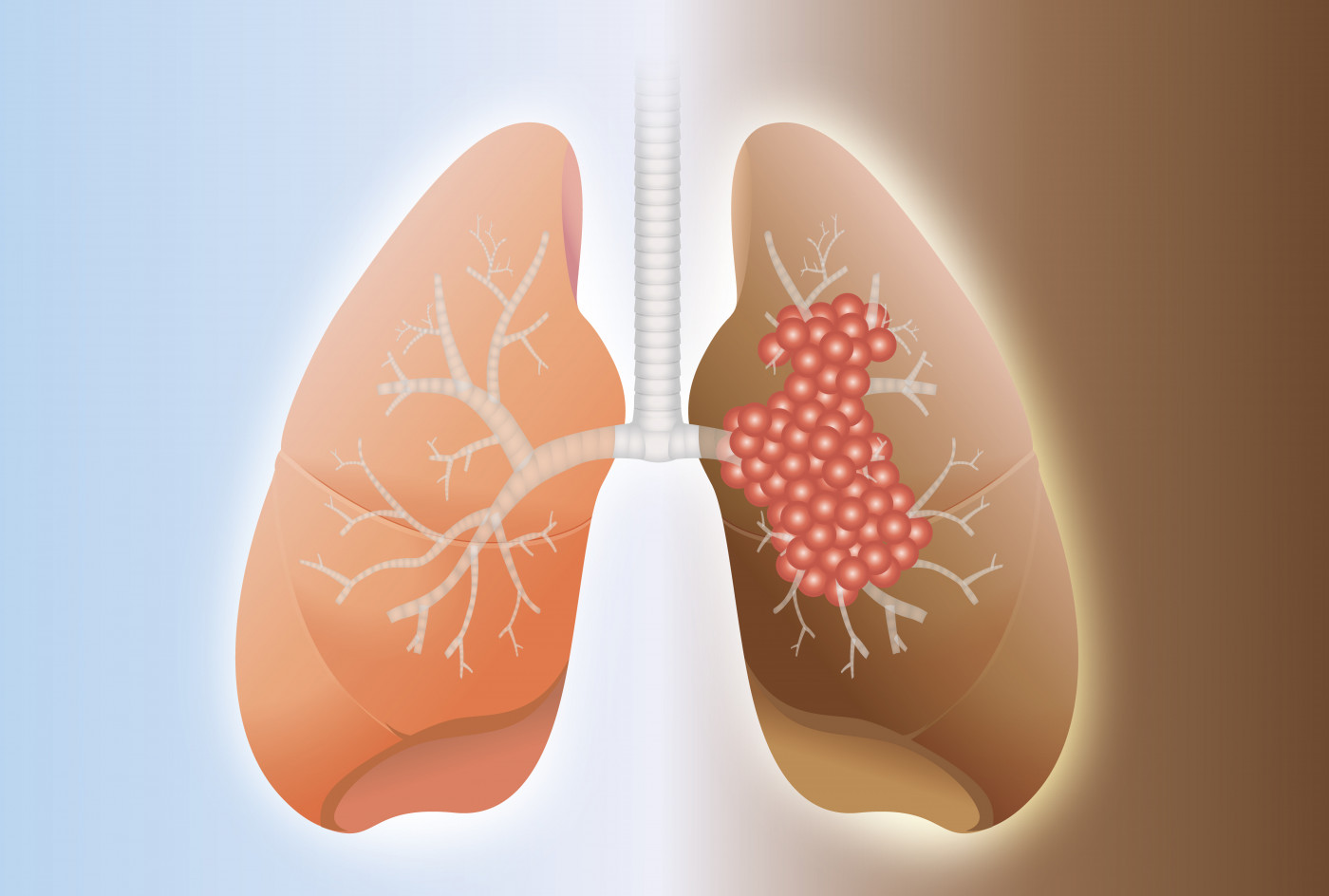
Nearly one in every two people with advanced lung cancer also have pulmonary arterial hypertension, a study published in the journal Science Translational Medicine reports.
The study, “Lung cancer–associated pulmonary hypertension: role of microenvironmental inflammation based on tumor cell-immune cell crosstalk,” showed that lung cancer progression leads to remodeling of blood vessels, and consequently the development of pulmonary arterial hypertension. This knowledge can help physicians to better understand respiratory symptoms of lung cancer and improve patients’ care.
Lung cancer is responsible for about 28 percent of all cancer-related deaths worldwide. These patients are at twice the risk of developing secondary respiratory and cardiovascular diseases, which are believed to contribute to shortness of breath and respiratory distress. But little is known about the origin of these secondary diseases.
Researchers at the Max Planck Institute for Heart and Lung Research (MPI-HLR) in Bad Nauheim and the German Center for Lung Research analyzed high-resolution computed tomography (CT) images of 519 people with advanced lung cancer.
They found that 250 patients — about 48 percent — had a pulmonary artery diameter greater than 28 mm, highly suggestive of pulmonary hypertension.
“We found thickening of the walls of the pulmonary artery in more than half the patients. This is a clear indication that these patients also suffer from pulmonary hypertension,” Rajkumar Savai, principle investigator at MPI-HLR and senior author of the study, said in a university news release.
Additional evaluation of the mean pulmonary artery systolic pressure (mPASP) of 70 of these patients further supported a pulmonary hypertension diagnosis, with values ranging between 33 and 70 mmHg. About 46 percent had a mPASP above the normal cutoff of 34 mmHg.
Analysis of 14 lung tissue samples confirmed the remodeling of blood vessels with increased vessel wall thickness, a hallmark of pulmonary hypertension.
To better understand how pulmonary hypertension correlates with the development of lung cancer, the team used three different mice models — each develops cancer at a different rate, allowing a more detailed view into how cancer and its symptoms develop.
Analysis of lung tissue collected from these animals revealed that cancer cells were not responsible for pulmonary hypertension but the immune cells they recruit were. Indeed, macrophages and T-cells were found to infiltrate vessel walls and release pro-inflammatory signaling molecules that, in turn, trigger both cancer cell migration and resistance, and vessel remodeling.
“Previously unknown abnormalities in blood vessels, triggered by inflammatory processes in lung tumors, could be the underlying cause of the symptoms observed in patients,” said Werner Seeger, director of the Max Planck Institute and of the Medical Unit at Giessen-Marburg University Hospital.
The researchers believe that immune and inflammatory processes triggered by cancer cells might be the cause of pulmonary hypertension development, and that specifically targeting the identified pro-inflammatory mechanism may help manage the lung cancer-associated pulmonary arterial hypertension, improving a patient’s symptoms and outcome.



