HRCT Predicts Lung Function Decline in SSc Patients
Written by |
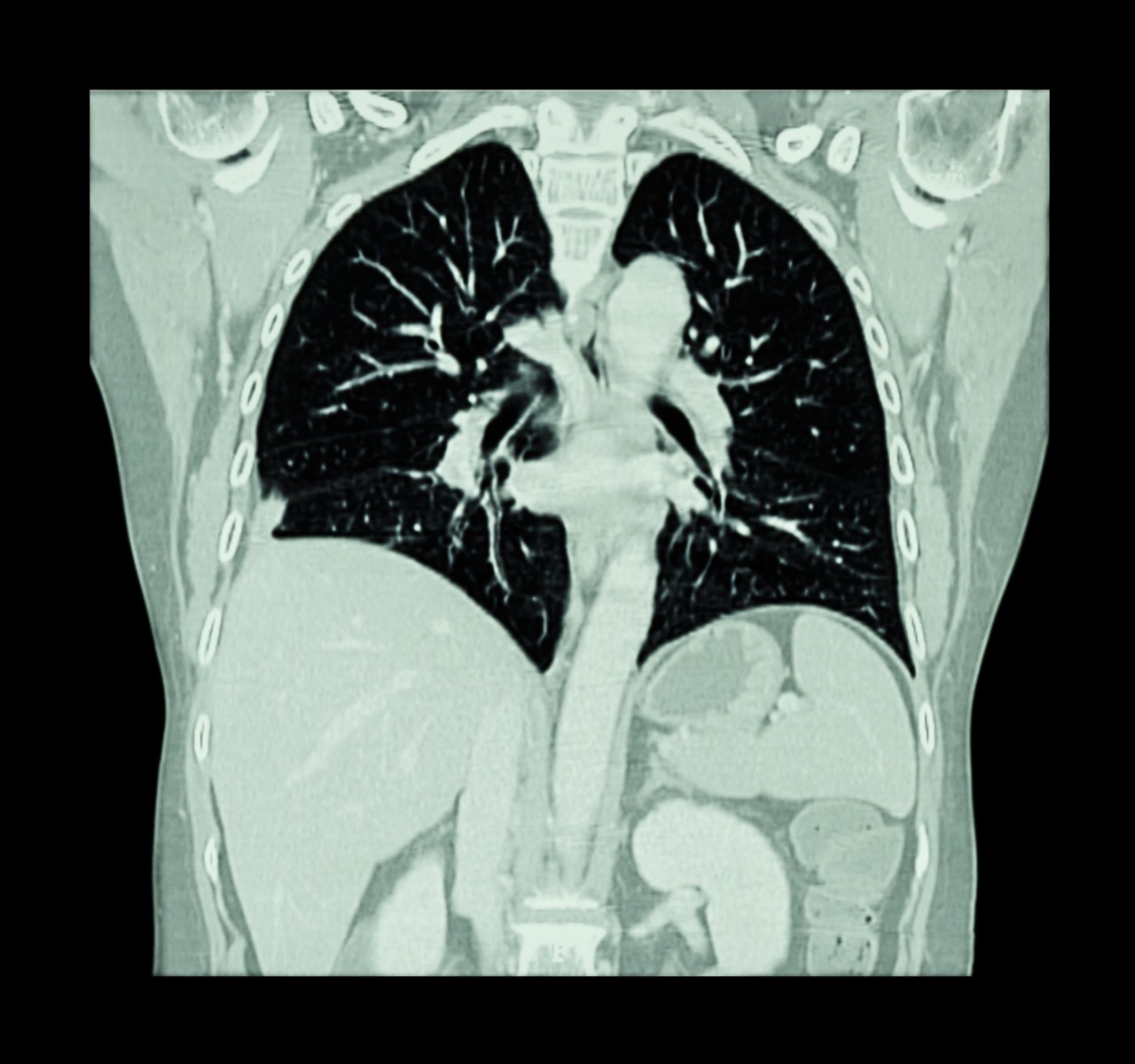
Patients with systemic sclerosis (SSc) are at an increased risk for mortality due to concurrent pulmonary hypertension or interstitial lung disease. While pulmonary hypertension results in right-sided heart failure, interstitial lung disease results in extensive lung fibrosis. It may be possible to test for lung scarring using high resolution computed tomography (HRCT) imaging, and a group of researchers from the Department of Rheumatology at Oslo University Hospital in Oslo, Norway, found a high predictive capacity of imaging on lung function.
“Here, detailed, serial lung fibrosis measurements and paired pulmonary function tests (PFTs) were assessed as outcome prediction tools in a prospective SSc cohort,” stated the authors in the manuscript, “Predictive Value of Serial HRCT Analyses and Concurrent Lung Function Tests in Systemic Sclerosis,” which was published in the journal Arthritis & Rheumatology. The goal of the study was to enable identification of risk for SSc-associated interstitial lung disease at an early stage before extensive lung fibrosis reduces the quality of life for the afflicted patient.
Since pulmonary function test parameters are not specific to interstitial lung disease, the authors chose to couple tests with HRCT, which is an imaging modality with sensitivity much higher than that of X-rays. Using these methods, the authors were able to answer five key questions, including: “What is the frequency of interstitial lung disease in SSc over time? What is the predictive value of baseline HRCT for fibrosis progression and lung function?”
Focusing on the first question, the researchers identified 305 patients who met the 2013 ACR/EULAR SSc classification criteria. These patients had available HRCT images and pulmonary function tests. At first presentation at the clinic, there was a mean lung fibrosis extent of 6.8% that eventually progressed to 8.4% at follow-up. The majority (65%) of patients had lung fibrosis, while the remaining had no signs of lung fibrosis–this did not change, even at the time of follow-up.
Additionally, the authors determined that baseline HRCT correlates well with lung function. Individuals with greater than 20% baseline fibrosis evident from HRCT had the lowest forced vital capacity (FVC) percent. Those patients with the worst fibrosis had greater than a 10% decline in FVC at follow-up.
“These prospective cohort data suggest that HRCT performed at baseline predicts fibrosis development, rate of fibrosis progression and pulmonary function decline in SSc,” concluded the authors. Although the study was limited by the variable follow-up periods between patients, the study was able to make a connection between HRCT and deterioration of lung function over time.



