Idiopathic PAH Vasodilator Response Reflects Blood Flow Problems
Written by |
 Patients with idiopathic pulmonary arterial hypertension (PAH) who responded to an acute vasodilator challenge — a clinical test that can predict how severe the disease will become — had fewer baseline blood flow abnormalities compared with non-responders. The study appeared in a research letter published in Annals of Internal Medicine, titled “Acute Vasodilator Responsiveness and Microvascular Recruitment in Idiopathic Pulmonary Arterial Hypertension.”
Patients with idiopathic pulmonary arterial hypertension (PAH) who responded to an acute vasodilator challenge — a clinical test that can predict how severe the disease will become — had fewer baseline blood flow abnormalities compared with non-responders. The study appeared in a research letter published in Annals of Internal Medicine, titled “Acute Vasodilator Responsiveness and Microvascular Recruitment in Idiopathic Pulmonary Arterial Hypertension.”
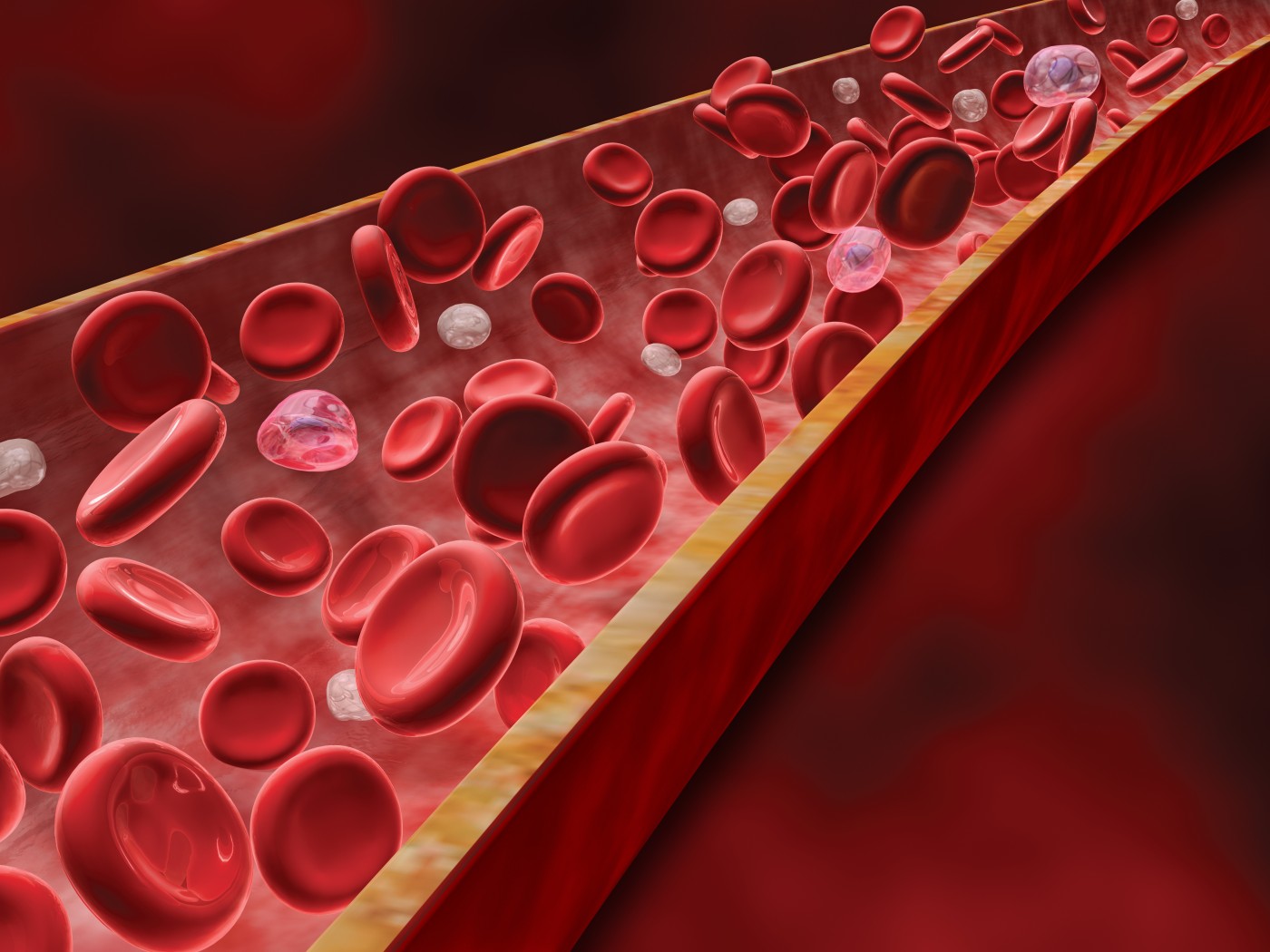
Pulmonary arterial hypertension (PAH) refers to high blood pressure of the lungs. PAH is a chronic and can cause right heart failure if it is not treated.
[adrotate group=”4″]
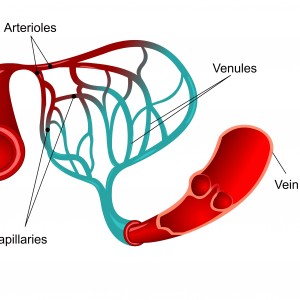
Acute vasodilator testing is used to measure how much the pulmonary blood vessels relax over a short time period. The test involves giving a patient a medication that will dilate blood vessels, such as intravenous epoprostenol, intravenous adenosine or inhaled nitric oxide. The test can be used to screen for patients who could respond to calcium channel blockers, but can also be used to determine how the disease will progress. The prognosis is better for patients who have vasodilator responses than it is for non-responders. Blood flow (hemodynamic) abnormalities might help to indicate who can respond to this test and who will not.
Lead author David Langleben, MD, from McGill University, Montreal, and his co-workers wrote, “Despite sharing the baseline hemodynamic profile of [idiopathic] PAH, responders and nonresponders represent different vascular phenotypes and perhaps different diseases.”
The scientists tested 14 patients with idiopathic PAH who had not received idiopathic PAH-specific therapy using an acute vasodilator challenge.
During this challenge, the right heart is catheterized, meaning a tube is inserted into the femoral artery of each patient. After 30 minutes, they took baseline hemodynamic measurements, then they assessed the activity of pulmonary capillary endothelium-bound (PCEB) angiotensin-converting ectoenzyme (ACE) activity, which is a test for lung function and injury.
They performed the acute vasodilator challenge using intranvenous epoprostenol. Two people responded to the test and twelve did not.
[adrotate group=”3″]
In the 12 nonresponders, there was no change in the pulmonary arterial pressure, the output of the heart increased and pulmonary vascular resistance decreased, but in the two responders the average pulmonary arterial pressure increased.
The non-responders had measurable blood flow abnormalities at baseline, such as a low functional capillary surface area which did not increase at the highest dose of the vasodilator epoprostenol. Responders had a higher functional capillary surface area at baseline, which increased greatly at the highest dose of epoprostenol. Capillary surface area helps to facilitate exchange of nutrients and other molecules between the blood and tissues.
The researchers concluded that the responders may “accommodate the increased cardiac output by true microvascular recruitment … this group can achieve normal levels of lung perfusion.”
The improved blood flow in the responders could help to compensate for this lung disease. Both blood flow abnormalities and the vasodilator challenge could be used to predict the outcomes of PAH, and may help guide the selection of treatments for this disease.



