Skeletal muscle dysfunction not cause of reduced exercise capacity
Finding stems from recent research on rat models of PH
Written by |

Reduced exercise capacity appeared to be a consequence of cardiac and pulmonary changes, but not skeletal muscle alterations, in rat models of pulmonary hypertension (PH), according to recent research.
While no functional problems with muscles could be observed despite obvious impairments in exercise capacity, significant cardiopulmonary dysfunction was already present.
“This study provides direct evidence showing reduced exercise capacity in PH occurs before skeletal muscle dysfunction and suggesting that intrinsic changes in skeletal muscle are not causative to exercise intolerance in PH,” the study’s researchers wrote in “Reduced exercise capacity occurs before intrinsic skeletal muscle dysfunction in experimental rat models of pulmonary hypertension,” which was published in Pulmonary Circulation.
Exercise intolerance is a main symptom of PH, wherein patients’ ability to be physically active is reduced. This disease feature is an important indicator of prognosis, with a lower exercise capacity early on predicting worse outcomes later.
This diminished capacity is largely regarded as a consequence of the cardiac and lung impairments, along with poor circulation, that mark PH.
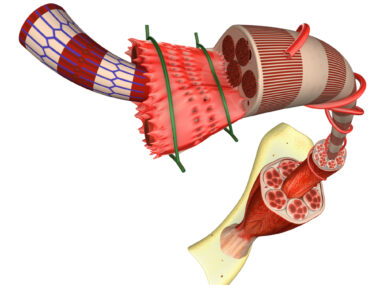
Recently, some evidence suggested that dysfunction of the skeletal muscles, which connect to bones and enable voluntary movements, could also be involved. Various changes in skeletal muscles, including atrophy (wasting), reduced speed and strength of muscle contractions, and impaired function of mitochondria — the cellular organelles that produce energy — among others, have been observed in PH patients and animal models.
Evaluating exercise capacity in PH rat models
Here, scientists looked at exercise capacity, heart function, and skeletal muscle function in two rat models of PH to better understand the relationship between skeletal muscle dysfunction and reduced exercise capacity in PH, and to learn whether skeletal muscle problems might directly contribute to a reduced ability to be physically active.
The models, each created using a different strain of rats, represent different PH severities. The Sprague-Dawley (SD) model is relatively less severe than the Fischer (CDF) model, where cardiopulmonary dysfunction and death occur sooner.
In the SD model, the rats developed dysfunction of the heart’s right ventricle (RV), which is responsible for pumping blood from the heart to the lungs, compared with healthy rats. This was accompanied by significant reductions in oxygen uptake during exercise, an indicator of reduced exercise capacity.
The rats didn’t show any changes in skeletal muscle mass, mitochondrial function, muscle force, or muscle fatigue in the soleus muscle of the leg, a major muscle used by rats during exercise.
In the more severe CDF model, signs of RV dysfunction and reduced exercise capacity were again observed. Unlike their less severely affected counterparts, these rats did show signs of muscle atrophy and levels of proteins related to mitochondria and cell metabolism were altered compared with healthy animals.
Still, there were no functional alterations in muscle force, fatigue, or mitochondrial function, despite the impairments in exercise capacity.
Altogether, the evidence suggests that reduced exercise capacity in these rat models arises before skeletal muscle dysfunction and, therefore, “intrinsic alterations in skeletal muscle are not causative to exercise intolerance in PH,” the researchers wrote.
Instead, the results support the existing theory that the symptom directly arises from cardiopulmonary factors. For this reason, “improving central cardiopulmonary impairments including RV function (particularly at the early stage of PH) may be critical in preventing or delaying the occurrence of exercise limitation in settings of PH,” they wrote. “Most importantly, there remains an urgent unmet need to therapeutically target RV dysfunction to improve PH prognosis and exercise capacity.”