Researchers Show How Microvasculature is Involved in CTEPH Pathogenesis
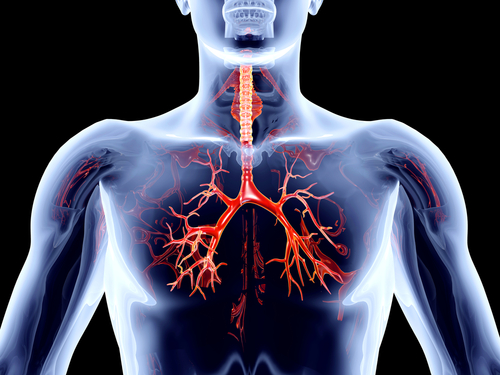
 Patients with chronic thromboembolic pulmonary hypertension (CTEPH) who respond differently to treatment with pulmonary endarterectomy (PEA) may have differences in microvascular structure. When a team of researchers from Paris-South University and Centre Chirugical Marie Lannelongue investigated CTEPH pathogenesis in humans, they applied their findings related to microvasculature changes to generate an animal model of CTEPH that sufficiently reproduced the disease.
Patients with chronic thromboembolic pulmonary hypertension (CTEPH) who respond differently to treatment with pulmonary endarterectomy (PEA) may have differences in microvascular structure. When a team of researchers from Paris-South University and Centre Chirugical Marie Lannelongue investigated CTEPH pathogenesis in humans, they applied their findings related to microvasculature changes to generate an animal model of CTEPH that sufficiently reproduced the disease.
As reported in “Microvasculature Disease in CTEPH: A Role for Pulmonary Veins and Systemic Vasculature,” microvasculature, or tiny blood vessels, can be remodeled in the pathogenesis of CTEPH, leading to blood shunting and clinical symptoms. The team made this finding through retrospective studies of clinical data and tissue samples from 17 CTEPH patients who had either undergone PEA and saw no improvements or could not undergo PEA due to inoperability.
[adrotate group=”4″]
The most striking characteristics of histological samples was the abundance of fibrosis around the majority of pre-capillary vessels. Seven out of nine ineffective PEA patients showed signs of fibrosis around small pre-septal venules and larger septal veins; all eight inoperable PEA patients showed signs of both.
An ink injection experiment, where the researchers injected blue and green dyes into separate blood vessels of a lung sample from an ineffective PEA CTEPH patient, revealed the existence of bronchopulmonary venous shunting. This shunting may have led to remodeling of vasculature and increased pressure in blood vessels.
[adrotate group=”3″]
As a potential contributor to pulmonary hypertension, it is important to understand microvascular disease. To further understand how clinical findings of microvasculature remodeling relate to CTEPH pathogenesis, the team induced CTEPH in piglets through post-embolic pulmonary hypertension. Histology showed severe septal vein remodeling, venous lesions, and occluded arterials in all animals.
The authors stated the impact of their study as “confirm[ing] the importance of small vessel or microvascular disease in lungs from inoperable patients or with persistent pulmonary hypertension after PEA.” Considering the clinical impact, however, an editorial commentary from University of California San Diego, “Microvascular Disease in Chronic CTEPH: The Story Continues,” believes “that these observations required further investigation,” and that the study “raises yet more questions that it seems to answer.” However, it was noted that this is a hallmark of all important observations, indicating the study may have greater clinical relevance with time and additional experimentation.